Regarding inquiries about fungal ailments, Andrej Spec, MD, has established himself as the primary authority for healthcare professionals globally. Each week, he receives between 10 and 15 calls from doctors seeking assistance with intricate fungal diagnoses or treatment issues. He has addressed inquiries from all over the United States and from as distant as China, Thailand, Japan, Australia, and Europe.
“The challenge is that numerous doctors were educated to perceive fungal infections as localized and uncommon,” remarked Spec, an associate professor of medicine in the Division of Infectious Diseases. “Thus, when patients present with indications of an infection, they often overlook the possibility of a fungal cause until all other options have been exhausted.”
This clinical oversight can lead to patients with fungal infections embarking on extensive and exasperating diagnostic journeys, which extend illnesses and deteriorate outcomes. The WashU Medicine Invasive Fungal Infections Clinic, founded in 2015, is making significant progress in reducing that journey and delivering exceptional diagnosis and treatment for this frequently neglected category of infectious diseases. Within its inaugural decade, the clinic has expanded from a solo specialist attending to three or four patients weekly to a bustling practice with three physicians, handling 1,200 patient visits annually and gaining an international reputation that attracts patients from 37 U.S. states and five countries. The clinic was designated a Center of Excellence, Diamond Level, by the European Confederation of Medical Mycology last year. It stands among only 13 clinics globally that have earned this honor, with only two located in the United States. The other is at MD Anderson Cancer Center, which exclusively treats MD Anderson patients and does not accept referrals.
“Achieving this acknowledgment is no simple feat,” stated Spec, the founding director of the WashU Medicine fungal clinic. “You must demonstrate excellence in three key areas: diagnosis and testing; patient care; and research. Patients seek us out only when they have exhausted their options elsewhere.”
Surviving scopulariopsis

Jonathan Ferretti, a 22-year-old resident of St. Louis, feels fortunate that the WashU Medicine fungal clinic was conveniently located when he fell ill with one of the rarest and most deadly fungal infections. In 2020, as he was receiving treatment for aggressive leukemia at St. Louis Children’s Hospital, dark spots began to surface on his body, initially on his knee, followed by his back. Effectively treating Ferretti’s leukemia involved targeting the same immune cells responsible for combating infections, and the unusual spots immediately drew the attention of Ferretti’s medical team, including WashU Medicine pediatric oncologist Shalini Shenoy, MD, and pediatric infectious disease expert Rachel Orscheln, MD. Both physicians are professors of pediatrics who attend to patients at St. Louis Children’s Hospital.
They consulted Spec for an evaluation, and he arrived at the diagnosis: the spots were a manifestation of Scopulariopsis, a fungal organism from the soil that had exploited Ferretti’s weakened immune system to infiltrate his bloodstream and disseminate throughout his body.
At that point, only a few dozen instances of disseminated scopulariopsis disease—characterized by its spread throughout the body—had been documented in medical literature. All reported cases had proven fatal.
“By the time I developed scopulariopsis, I had endured chemotherapy, radiation, intubation, and a stem-cell transplant for leukemia,” Ferretti recounted. “My mindset had become so skewed due to cancer treatment that I failed to comprehend the severity of this fungal infection. I merely viewed it as another hurdle to manage.”
Prior to the initiation of his intensive cancer therapy, his healthcare providers had proactively prescribed three leading antifungal medications to prevent such infections; however, none were effective against the encroaching scopulariopsis. With no FDA-approved treatments specifically available for disseminated scopulariopsis and the infection progressing swiftly, Spec identified that Ferretti’s sole chance for survival lay in participating in a clinical trial for the experimental antifungal agent olorofim, developed by the biotechnology firm F2G. Spec and his team hastened to secure Ferretti’s enrollment in the trial and to commence treatment.
Within weeks, the dark spots began to fade, although more than a year passed before Spec felt assured in discontinuing the medication for Ferretti. The trial has since completed, and F2G is currently in the process of seeking FDA approval for olorofim.
“When Dr. Spec informed me that I might be the first individual to survive disseminated scopulariopsis, I was astounded,” said Ferretti. “I still find it difficult to believe.”
Expanding expertise beyond WashU Medicine
Ferretti represents one of thousands whose lives have been transformed by the Invasive Fungal Infections Clinic. The clinic has established its reputation by offering advanced diagnostics and cutting-edge treatment for various fungal infections, with a particular focus on Histoplasma, a soil fungus that leads to histoplasmosis, an illness characterized by flu-like symptoms such as fever, cough, and chills. However, histoplasmosis is considerably more perilous than influenza. In general, the fungus is lethal to about 5% of individuals who contract it, and the mortality rate escalates to 30% or higher for those with weakened immune systems.
This mold is found worldwide, but its most significant concentration is in the Midwest, where WashU Medicine physicians and researchers have developed globally recognized expertise in identifying and treating histoplasmosis. The WashU Medicine clinic also boasts what may be the only multidisciplinary care team specializing in a rare yet severe and permanent complication of histoplasmosis known as fibrosing mediastinitis. In this condition, abnormal growth of tissues within the chest can obstruct airways, blood vessels, and the esophagus.
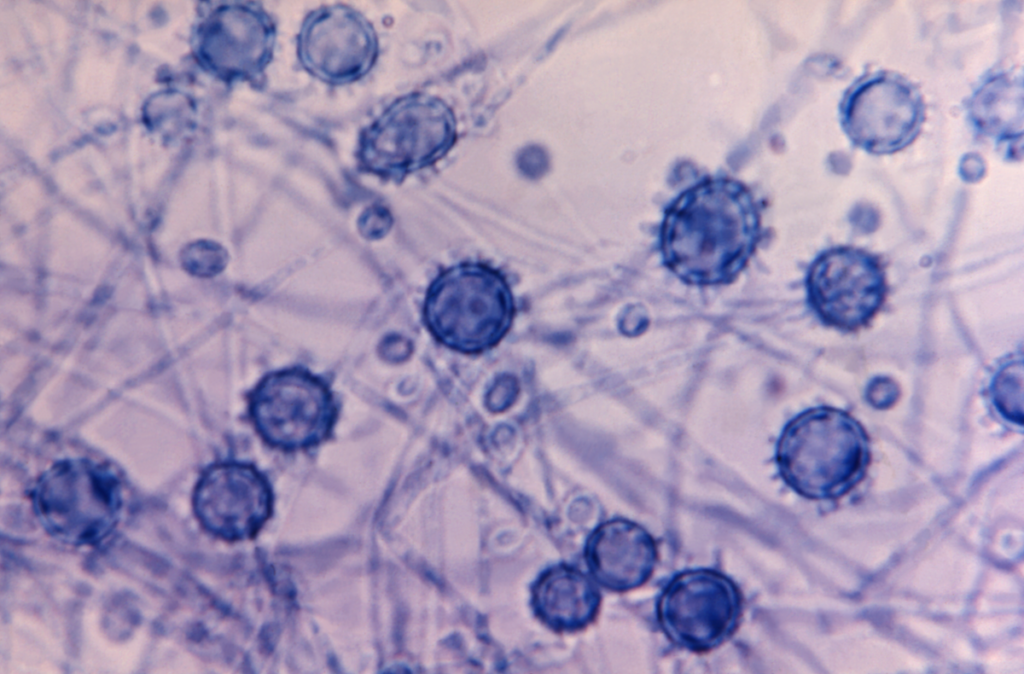
Moreover, the clinic is taking part in numerous clinical trials for alternative fungal infections. These trials can provide access to experimental treatments for individuals who have exhausted standard options. The physicians at the clinic also engage in research pertaining to fungal infections, with a concentration on Cryptococcus, Histoplasma, Candida, Aspergillus, and other invasive molds,including the epidemiology of these infections and elements influencing outcomes in infected individuals.
A majority of individuals suffering from invasive fungal infections encounter at least one erroneous diagnosis and ineffective treatment; across the nation, the average number of incorrect diagnoses among patients with fungal infections stands at four. Adriana Rauseo, MD, an assistant professor in medicine and part of the clinical team at the fungal clinic, is dedicated to streamlining the diagnostic process for patients by training primary-care providers to recognize fungal infections.
“To reduce the frequency of misdiagnoses, it is essential to enhance awareness of fungal infections beyond just infectious disease specialists,” Rauseo stated. “We need primary-care providers to begin to ‘think fungi.’ While it may not be feasible to achieve an average diagnosis on the first attempt, receiving a diagnosis by the second visit is far superior to the fifth. The intention is to start with local healthcare providers and then broaden our reach.”
As the institution hosting the fungal clinic, WashU Medicine is one of the rare facilities that can provide comprehensive training in diagnosing and managing invasive fungal infections. Infectious disease fellows from other institutions sometimes rotate through WashU Medicine specifically to gain experience in the fungal clinic.
The medical community must quickly catch up concerning fungi since the situation may be deteriorating. A 2022 study by Spec and colleagues indicated that lung infections caused by environmental fungi—once limited to specific regions in the U.S.— have become a national concern as certain species of pathogenic fungi have expanded beyond their traditional habitats in recent years, potentially due to climate change.
Even more concerning, new fungal pathogens are likely to emerge, as noted by Spec. Many fungi present in soil, water, and air possess the molecular mechanisms to cause disease in humans but infrequently do so, mainly because they thrive in cooler climates and struggle to survive at human body temperature. However, with rising global temperatures leading to extended and hotter heatwaves, environmental fungi are compelled to adapt to elevated temperatures. Fungi may become problematic in a warmer climate.
Collaboration with patients enhances care
Patrick B. Mazi, MD, an assistant professor of medicine and a key member of the fungal clinic’s faculty, serves on the board of the fungal patient advocacy organization Mycology Advocacy, Research & Education, or MyCARE. Co-founded by Spec in 2023 alongside patient activist Rob Purdie and medical education expert Lisa Tushla, MyCARE aims to enhance the diagnosis and treatment of fungal infections by driving awareness, assisting patients and their caregivers, and advocating for increased and improved research.
“Rob Purdie often says, ‘I was diagnosed using a test that’s 50 years old, and receiving treatment with a medication that’s 70 years old. No other medical diagnosis would ever accept that,’” Mazi remarked. “He’s absolutely correct! To effectively manage invasive fungal infections, we require improved diagnostics and superior treatments, which underscores the need for research.”
Clinical mycology, which relates to the scientific investigation and treatment of fungal infections, is significantly underfunded compared to other domains of disease research, compelling fungal researchers to think creatively. They are now consulting with patients like Purdie to steer research in ways that will have the most substantial impact on the lives of those affected.
“I must confess that I was somewhat taken aback when I first conversed with patients and caregivers about their priorities,” Mazi noted. “I initially assumed that better treatments would be the foremost concern for everyone. However, most patients emphasize the need for improved diagnostics so they could have received their diagnoses and treatments more swiftly. This indicated to me that their experiences during the early stages of their fungal infection journeys were so distressing that even years later, they preferred to rectify that for future patients rather than seek improved treatments for themselves.”
Currently, Ferretti is a largely healthy 22-year-old college student with aspirations of pursuing a career in pediatric oncology nursing. He experiences some residual effects from his cancer treatment but has fully recovered from his encounter with one of the world’s deadliest fungi. He and his mother participated in MyCARE’s inaugural meeting in May 2023 held in Denver, where one of the co-founders is located.
“This conference truly opened my eyes to the potential severity of fungal infections,” Ferretti shared. “It was honestly frightening. Some individuals endured extensive hardships before receiving the necessary treatment. Despite having experienced an invasive fungal infection myself, I didn’t fully grasp how dire it could be until I attended that event. I consider myself fortunate to have had Dr. Spec on my team from the outset. He literally saved my life.”
About Washington University School of Medicine
WashU Medicine is a preeminent institution in academic medicine, encompassing biomedical research, patient care, and educational initiatives, supported by 2,900 faculty members. The National Institutes of Health (NIH) research funding portfolio of WashU Medicine ranks as the second largest among U.S. medical schools, having increased by 56% over the past seven years. Together with institutional investments, WashU Medicine allocates over $1 billion annually to innovation and training in basic and clinical research. Its faculty practice is consistently among the top five in the nation, with over 1,900 faculty physicians serving at 130 locations and also acting as medical staff at Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine boasts a rich history in MD/PhD training, having recently dedicated $100 million to scholarships and curriculum revitalization for its medical students, and offers outstanding training programs across all medical subspecialties, including physical therapy, occupational therapy, and audiology and communication sciences.
Originally published on the WashU Medicine website
The post WashU Medicine fungal specialists combat frequently misdiagnosed infections first appeared on The Source.

