“`html
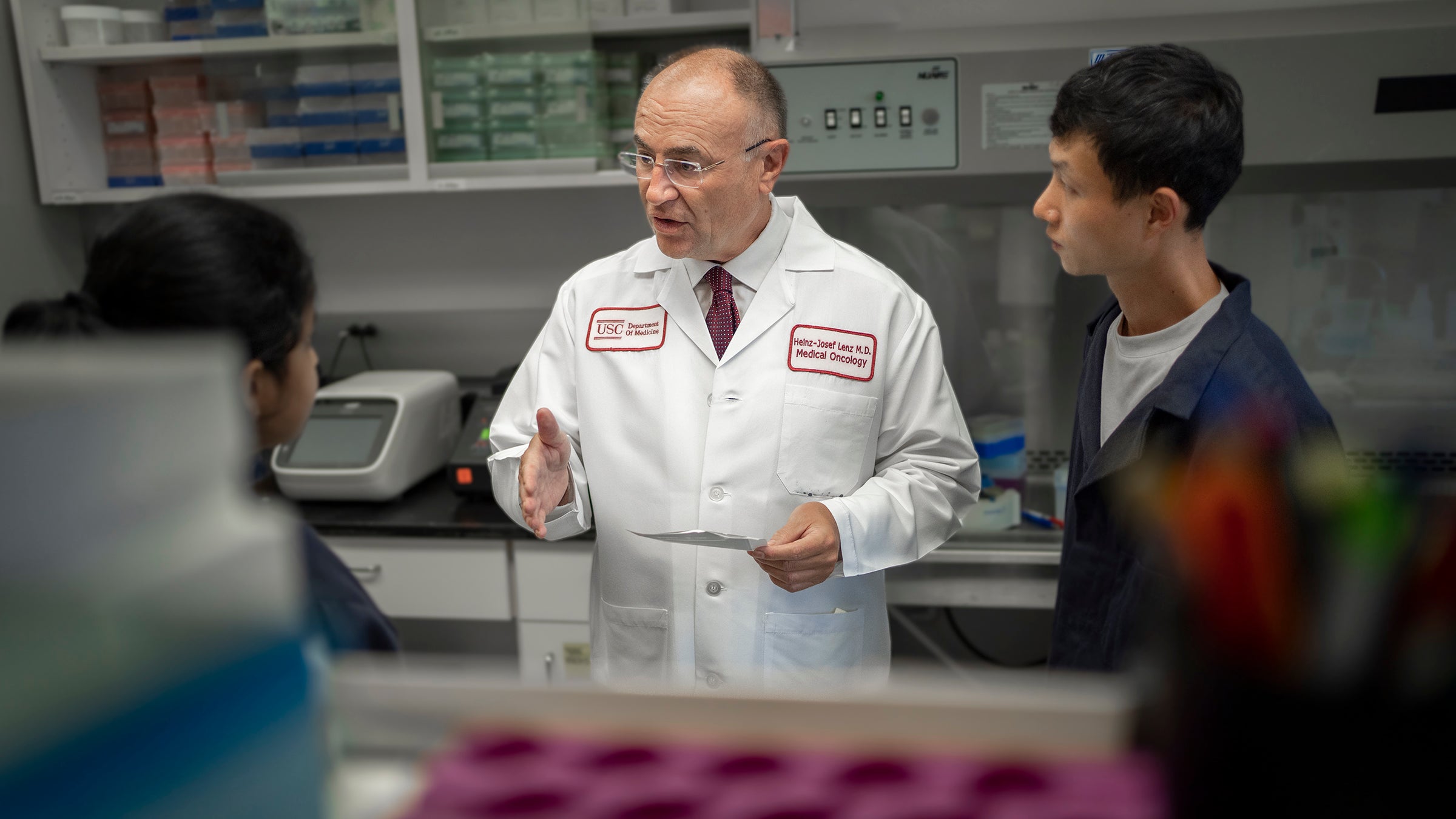
Heinz-Josef Lenz, in the middle, converses with postdoctoral researcher Pooja Mittal, on the left, and lab technician Jae Ho Lo. (Photo/Chris Shinn)
Health
USC investigators spearhead lifesaving advancements in cancer research
From laboratory to patient care, USC’s spirit of innovation promotes pioneering methods for detecting, treating, and preventing cancer.
A few years ago, Heinz-Josef Lenz, an esteemed professor of medicine and cancer biology at the Keck School of Medicine of USC and the J. Terrence Lanni Chair in Gastrointestinal Cancer Research, made an unexpected finding regarding colon cancer. He and his research group discovered that circadian rhythm — the body’s internal clock — affects the efficacy of colon cancer therapies, including immunotherapy and targeted antibodies.
Curious whether the circadian clock might be a new factor in combating colon cancer, Lenz endeavored to investigate this regulator of sleep-wake patterns. He soon recognized that one of the world’s leading specialists on the circadian clock, Steve Kay, was also a faculty member at the Keck School of Medicine.
Despite Kay — a University and Provost Professor of Neurology, Biomedical Engineering, and Quantitative and Computational Biology; the David L. Lee and Simon Ramo Chair in Health Science and Technology; and director of Convergent Bioscience — lacking expertise in colon cancer, he was enthusiastic when Lenz reached out to collaborate. Their respective laboratories began a vigorous exchange of insights.

“What we discovered is that several circadian clock proteins our lab has been investigating for many years act as the ‘accelerator’ to cancer,” Kay noted. “This led to a series of experiments that truly astonished all of us. Drugs my lab created to target the circadian clock demonstrated the ability to eliminate colorectal cancer cells.”
Lenz and Kay are part of a larger group of USC researchers achieving lifesaving innovations in cancer detection, prevention, and treatment through creative thinking, groundbreaking technology, and interdisciplinary collaboration. Their partnership, like many others at USC, was born out of the university’s distinctive research environment, which set the stage for their achievements.
A spirit of innovation
The two researchers exemplify the vast spectrum of cancer-fighting knowledge represented across USC’s health sciences schools, centers, and hospitals. These encompass the Keck School of Medicine, the Keck Medicine of USC health system, the USC Norris Comprehensive Cancer Center, the USC Norris Cancer Hospital, the USC Alfred E. Mann School of Pharmacy and Pharmaceutical Sciences, the USC Leonard Davis School of Gerontology, and Children’s Hospital Los Angeles, among various others. Regular collaborators include scientists at the USC Viterbi School of Engineering and the USC Dornsife College of Letters, Arts, and Sciences.
A university-wide focus on translational research (bridging findings from the lab into practical applications…
“““html
Applications) and integrative science (uniting specialists from varied disciplines to address intricate challenges) fosters a culture of creativity. The Translation and Clinical Sciences Program at the USC Norris cancer center, for instance, brings together scholars from five schools and 18 departments to explore and develop groundbreaking therapies and biomarkers aimed at enhancing clinical results for cancer sufferers.
“The advantage of our health sciences institutions and services is that we have gathered some of the leading experts in the nation committed to preventing and managing cancer,” stated Steven Shapiro, USC’s senior vice president for health affairs. “Combining the extensive talent and scientific research we possess, paired with our enthusiasm for exploration, we will persist in promoting cancer advancements that will advantage our patients, community, and the globe.”
Lenz and Kay initiated their colon cancer research with funding from the USC Norris cancer center and subsequently broadened their studies to encompass breast cancer and liver cancer. A 2023 research by Kay, Lenz, and their associates demonstrated how liver cancer cells exploit circadian clock mechanisms to proliferate and disseminate. This work also guided Kay’s creation of a circadian clock-targeting compound for glioblastoma, a lethal type of brain cancer — the first substance of its nature proven safe and effective in humans. A similar drug targeting the clock for colon cancer is currently underway. The team is partnering with Synchronicity Pharma Inc., a biotech firm founded by Kay, to make these compounds available on the market.
Continue reading to discover more innovative cancer advancements from USC researchers.
Overcoming brain tumors with electrical signals
Donning a cap equipped with electrodes for brain cancer treatment may resemble a scene from a science fiction narrative. However, a research group led by USC’s David Tran has found that such a device — termed Tumor Treating Fields (TTFields) — might present new possibilities for glioblastoma patients.
As stated by the National Brain Tumor Society, the average survival for individuals diagnosed with glioblastoma — a highly aggressive and challenging brain tumor — is eight months. A recent investigation by Tran and his team indicated that the combination of chemotherapy and immunotherapy with TTFields correlates with a 70% enhancement in overall survival.
TTFields therapy administers precise waves of electrical fields directly into glioblastoma tumors via electrodes strategically placed on the scalp. Low-intensity alternating electric fields apply forces on vital structures within tumor cells, continually shifting their orientation.
“The TTFields apparatus cultivates an environment within tumor cells that imitates viral infection,” remarked Tran, associate professor of neurological surgery and neurology at the Keck School of Medicine, chief of neuro-oncology at Keck Medicine of USC, and co-director of the USC Brain Tumor Center. Tran has been investigating the therapy for over a decade.
These cellular alterations instigate a strong immune response within the tumor, bypassing its usual defenses against the body’s immune activities. Incorporating immunotherapy prevents the tumor from suppressing that immune reaction. “The immune system effectively performs the task of eliminating the tumor, which gradually diminishes over time,” Tran explained.
Remarkably, participants in the study with large, non-operable tumors survived even longer than those who had tumors surgically removed. “The larger the tumor,” Tran noted, “the greater the material available for an immune response” — a promising clue for patients whose tumors extend into highly sensitive parts of the brain, complicating surgical removal.
Tran is presently leading a significant international clinical trial for newly diagnosed glioblastoma to confirm the efficacy of TTFields in conjunction with immunotherapy and chemotherapy.
A cancer-combating compound from the ocean depths
Chemotherapy, a common cancer treatment, does effectively destroy cancer cells. However, it can also harm healthy cells in tissues like skin and hair, which are constantly proliferating and dividing, resulting in severe and often long-lasting side effects.

A groundbreaking investigation co-authored by Ryo Sanabria, an assistant professor of gerontology at the USC Leonard Davis School, has discovered a molecule that seems promising as a cancer treatment that may safeguard healthy cells while eliminating malignant ones. The molecule, known as mycothiazole (MTZ), originates from a unique source: sea sponges residing in the depths of the ocean.
Sanabria and Naibedya Dutta, a postdoctoral research fellow in the Sanabria Lab, collaborated with chemist and deep-sea diver Tyler Johnson, an associate professor of chemistry at Dominican University of California, to investigate MTZ’s impacts on human cells. When they applied MTZ to various human cancer cells — including liver carcinoma, breast cancer, and glioblastoma — the molecule obstructed the cells’ capacity to produce energy. Up to 80% of the cancerous cells treated with MTZ perished.
However, when MTZ was applied to healthy, non-malignant cells, the molecule had minimal impact. “It was astonishing,” Sanabria remarked. “Typically, when any drug is administered to any type of cell, you observe at least some gene expression alterations. But in healthy cells, we observed none.”
The research team also evaluated a synthetic variant of MTZ known as 8-O-acetylmycothiazole (8-OAc), which demonstrated similar findings. 8-OAc boasts a significantly longer shelf life compared to MTZ, making it potentially more appropriate for clinical applications. Future steps include testing the molecules in animal models and human participants.
A blood test for identifying ovarian cancer
Many cancers, such as breast cancer and skin cancer, are diagnosed through a tissue biopsy, wherein a small tissue sample is extracted using a needle. One exception is high-grade serous ovarian carcinoma (HGSOC), the most prevalent form of ovarian cancer.
Biopsy of a pelvic mass is deemed too hazardous since inserting a needle deep into the pelvis risks injuring critical organs and dispersing cancer cells into the abdominal cavity. Physicians normally perform surgery when they suspect HGSOC to remove a pelvic mass entirely. Nevertheless, invasive surgery carries its own risks, and research indicates that the vast majority of these masses are benign.
“““html
Bodour Salhia — associate professor of oncology biology at the Keck School of Medicine, holding the Royce and Mary Trotter Chair in Cancer Research, and serving as interim chair of the cancer biology department — along with her team, has created a straightforward blood assessment, or “liquid biopsy,” for HGSOC that might assist in identifying the cancer during its initial phases and spare numerous women from needless surgical procedures.
The assessment is grounded in Salhia’s investigations into cell-free DNA methylation. Methylation is an intricate alteration of DNA that can influence gene expression within the organism. “Cancerous cells exhibit modified DNA methylation profiles that we can detect in the bloodstream,” Salhia stated.
Salhia collaborated intimately with Lynda Diane Roman, associate professor of obstetrics and gynecology and head of the gynecologic oncology division at the Keck School of Medicine, along with other colleagues from the USC Norris cancer center to convert her genomics findings into a test that could bridge a clinical void in the diagnosis and management of HGSOC. A recent publication by Salhia, Roman, and their colleagues indicates that the blood test, termed OvaPrint, can ascertain whether a pelvic mass is benign or malignant with up to 91% precision.
OvaPrint is set to be commercially accessible later this year via the biotechnology firm Salhia founded, CpG Diagnostics Inc.
Fasting to enhance cancer treatment
Consuming a nutritious diet abundant in fruits, vegetables, legumes, and other plant-based foods can reduce cancer risk. Nevertheless, research by Valter Longo, professor of gerontology and biological sciences at the USC Leonard Davis School and the Edna M. Jones Chair in Gerontology, alongside his collaborators, has demonstrated that restricting food intake for brief periods can also be a formidable strategy in combating cancer.

For almost two decades, Longo’s laboratory has investigated how fasting and the “fasting-mimicking diet” (FMD) — a low-calorie, plant-centered regimen that mimics fasting for five days — influence cancer in mice. He discovered that fasting and FMD induce cellular and metabolic transformations that foster cancer prevention and treatment. These alterations create vulnerabilities in cancer cells that can be targeted by medications, enhance the efficacy of treatments like chemotherapy and immunotherapy, and safeguard healthy cells from the adverse effects of such therapies.
One of Longo’s recent discoveries, in partnership with the IFOM Cancer Institute in Milan, is that FMD becomes even more potent at treating specific cancer types in mice when paired with vitamin C. The amalgamation of FMD and vitamin C facilitates the destruction of cancer cells by prompting the body to generate an overabundance of reactive oxygen species, molecules that, at elevated levels, result in cell death. Previous research by Longo’s group indicated that FMD combined with chemotherapy amplifies immune system attacks on cancer cells.
Another recent investigation revealed that FMD enhances the tumor-fighting capabilities of hormonal therapies on breast cancer in mice and postpones drug resistance. Clinical trials imply that FMD may exhibit similar impacts in women battling breast cancer. Numerous trials in humans are presently exploring the effects of FMD in conjunction with various cancer-fighting pharmaceuticals, yielding promising early outcomes.
“I like to refer to FMD as the nontoxic wild card for cancer treatment,” Longo expressed. He aspires to a future where cancer is managed with low-toxicity “cocktails” such as FMD combined with vitamin C that eliminate cancerous cells while preserving normal ones.
Longo’s insights have been harnessed by his company L-Nutra to create FMD kits geared towards general health and customized for specific conditions including cancer, diabetes, and Alzheimer’s.
Innovative therapies for prostate cancer maintain quality of life
For men with intermediate-risk prostate cancer localized to the prostate, surgery and radiation are effective remedies, yet they carry the risk of undesirable side effects, such as erectile dysfunction, urinary incontinence, and bowel issues.
Researchers at USC Urology and the Keck School of Medicine are revolutionizing prostate cancer treatment with advanced focal therapy. This method targets only the portions of the prostate containing cancer cells, rather than excising the entire gland, thus minimizing side effects and preserving patients’ quality of life.
Andre Abreu, associate professor of clinical urology and radiology, along with Inderbir S. Gill — chairman and Distinguished Professor of Urology, the Shirley and Donald Skinner Chair in Urologic Cancer Surgery, and executive director of USC Institute of Urology — led a research group that was the first at an academic institution in the United States to examine focal high-intensity focused ultrasound ablation of the prostate as a primary approach to prostate cancer following FDA endorsement of the therapy. The procedure, which employs ultrasonic waves to heat and obliterate prostate cancer tissue, demonstrated a commendable success rate and minimal risk of impotence and incontinence.
“Focal therapy is increasingly becoming the favored treatment for men with organ-confined, intermediate-risk prostate cancer,” Gill commented. Other focal therapy modalities available at USC Urology comprise irreversible electroporation, which eradicates cancer using brief electrical bursts, and cryotherapy, which targets and eliminates prostate cancer cells utilizing extreme cold temperatures.
Presently, Abreu, who also directs image-guided surgery, focal therapy, and artificial intelligence for prostate cancer at Keck Medicine of USC, leads a national clinical trial assessing a water vapor system that utilizes specific amounts of steam to eliminate prostate tumors. Gill and Mihir Desai, professor of clinical urology, are pioneering Aquablation, an innovative robotic, high-pressure, high-precision water-jet device for eradicating prostate cancer cells from within the urethra. Serving as global co-principal investigators, they are directing an international, FDA-approved investigational device exemption (IDE) trial involving 280 men, comparing Aquablation with robotic radical prostatectomy surgery, the current standard.
“At USC Urology, innovation is our philosophy,” Gill mentioned.
“`