“`html
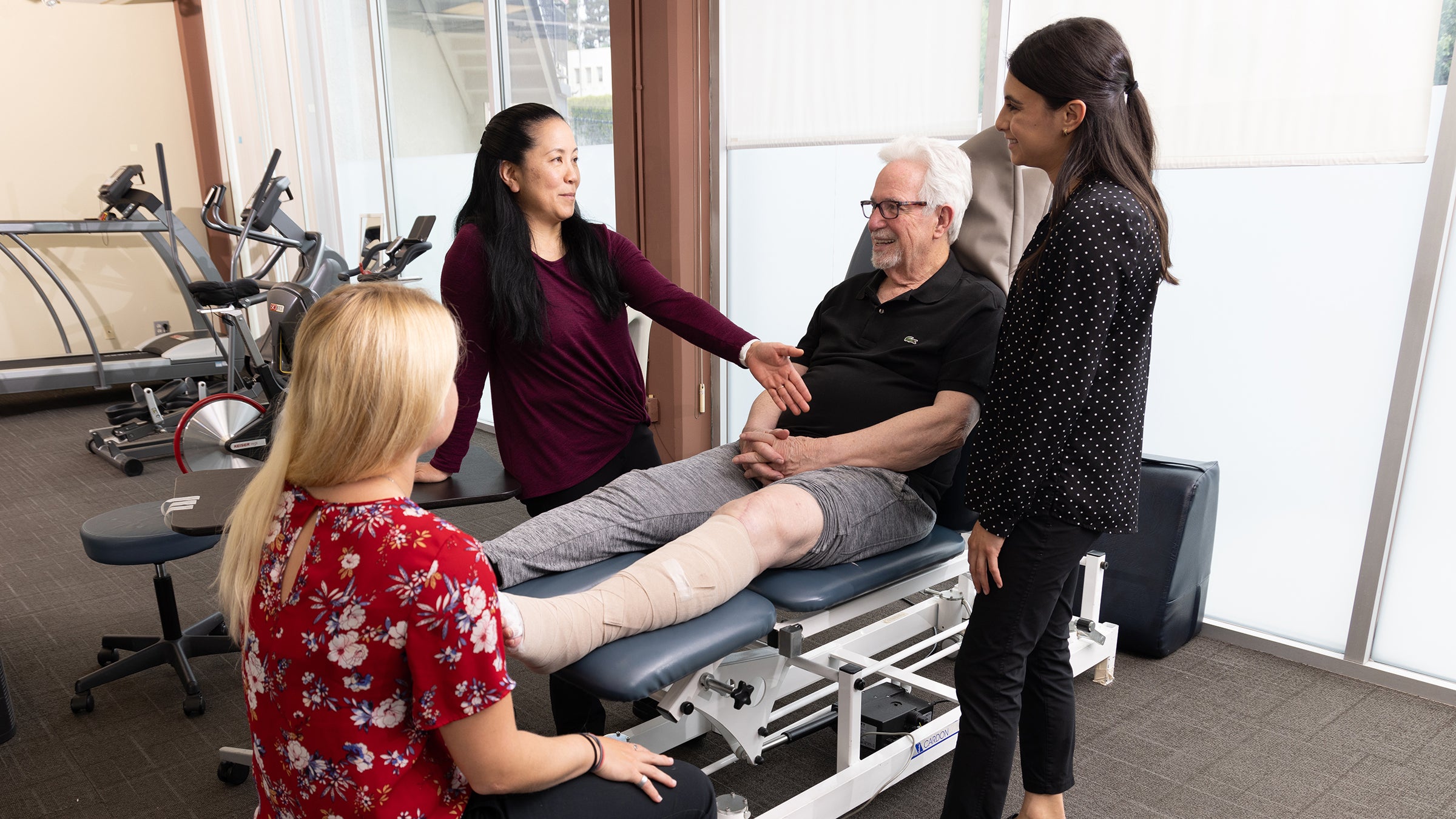
Kristine Kivuls, Kimiko Yamada, Duncan Wigg, and Lauren Vera, from the left, converse about Wigg’s progress. (Photo/Glenn Marzano)
University
USC cancer survivorship programs empower patients to thrive post-diagnosis
Cancer treatments are preserving and prolonging more lives than ever. USC professionals are assisting patients from diagnosis to treatment and navigating their post-care future by linking them with essential resources.
When Duncan Wigg, a 79-year-old retired psychologist and educator, experienced intense pain in his leg and hip in 2022, he had no reason to anticipate the diagnosis he would receive.
While his private practice orthopedic doctors initially believed he might require a hip replacement, one physician suspected something more serious could be behind the pain. A PET scan revealed a startling diagnosis: stage 4 lung cancer.
In the medical journey that ensued, that orthopedist referred Wigg to Keck Medicine of USC, where a multidisciplinary team of professionals would restore him to health — though not without challenges. Battling debilitating lymphedema (a fluid buildup common post-surgery and after cancer treatment) and muscle atrophy following surgery, Wigg acknowledges oncology physical therapist Kimiko Yamada and her team for assisting him in returning to his normal activities and a renewed state of health.
With cancer patients living longer than ever thanks to a series of innovative therapies and research advancements, USC practitioners are transforming post-diagnostic care to ensure survivors thrive in their new normal.
Through an interconnected network of survivorship programs, professionals from every sector of the university are directing patients from diagnosis to treatment and through their post-care journey by connecting them with the vital resources that enhance their chances for effective therapies and recovery. As patients survive for extended periods, and given the complexity of the cancer journey, practitioners collaborate across disciplines to ensure that no patient is overlooked or must navigate the journey alone.
“Her efforts to taper the swelling and assist me in regaining my strength were quite successful,” Wigg remarked of Yamada. “Keck Medicine’s coordinated and complementary care enabled me to overcome the repercussions of the illness and the surgery.”
An interconnected network of supporters
Yamada’s entry into oncology began early in her career, when a colleague at the USC Division of Biokinesiology and Physical Therapy had a list of cancer patients she needed to distribute. “I ended up working with her patients and fell in love with it,” shared Yamada, who is now an associate professor of clinical physical therapy and the director of the division’s oncology physical therapy residency program.
Yamada never returned the list and ultimately expanded her colleague’s practice, becoming a full-time oncology physical therapist and collaborating with a team of surgeons, medical oncologists, radiation oncologists, and specialists in speech and occupational therapy. “I don’t
“““html
“I believe I’ve discovered that level of collaboration at no other practice where I’ve been,” she remarked.
USC Physical Therapy boasts a cadre of oncology experts who assist cancer patients and survivors in enhancing their quality of life, alleviating pain associated with treatments, and addressing the distinct requirements of cancer survivors. The therapies provided encompass strategies for managing fatigue, lymphedema, and mobility issues; rehabilitation both pre- and post-surgery; exercises aimed at enhancing daily life activities; as well as strategies for minimizing stress and uplifting mood, among other services.
This initiative exemplifies how oncology professionals from USC’s health science schools and health system are delivering services aimed at enhancing quality of life. These services encompass mental health support for patients, survivors, and their caregivers, in addition to support groups designed to assist those who care for patients as they navigate the difficulties presented by a cancer diagnosis.
Survivorship commences at diagnosis
The concept of survivorship — which encompasses all individuals diagnosed with cancer as survivors — is an international standard for providers who support cancer patients.
“It was established to highlight that individuals diagnosed with cancer at any stage endure a multitude of traumas that extend beyond their health, touching upon financial burdens, family dynamics, social interactions, and future uncertainties,” stated Daphne Stewart, a medical oncologist at the USC Norris Comprehensive Cancer Center and a clinical professor of medicine at Keck School of Medicine of USC. Stewart also leads the women’s cancers section for medical oncology within the internal medicine department at the Keck School of Medicine.
“Individuals face immense pressure that we must recognize and address,” Stewart emphasized.
Within this framework, providers like Stewart consider how to collaborate with other professionals involved in cancer care, such as psychologists, social workers, exercise coaches, and nutrition experts, ensuring that patients can utilize all available resources within the health system.
Upon joining USC in 2023, Stewart initiated a clinical survivorship program for breast cancer patients who completed their primary treatment, which includes chemotherapy, surgical procedures, reconstruction, and radiation. Her team presently includes a medical oncologist, a nurse practitioner specializing in breast cancer, a social worker, and a nurse navigator.
Patients join the program to enhance their long-term mental and physical well-being while managing social and financial stresses, as noted by Stewart. After consulting with a nurse practitioner, patients may be referred to specialists in psychology, psychiatry, and physical therapy for therapies aimed at fostering mental and physical healing. This survivorship approach also focuses on weight management, blood sugar regulation, and regular monitoring to prevent future cancer occurrences. Moreover, for emotional and social support, the program features monthly peer meetings that provide a secure environment for patients to exchange experiences.
“It truly enables patients to discuss the significant stress stemming from the overall impact this has had on their lives,” Stewart explained. Patients speak about cancer-related changes, such as experiencing early menopause, chronic pain from treatments, body image issues, and other challenges.
Stewart recalls a patient who was vibrant, sociable, and self-sufficient prior to her breast cancer diagnosis. The ordeal was profoundly traumatic for her, as she received minimal support from friends and family.
“Joining the survivorship program was a profoundly positive step for her, as it provided the opportunity to cultivate a sense of community while also enabling her to envision a future beyond merely focusing on the side effects and the challenges she faced,” Stewart recounted.
“There are over 18 million cancer survivors in the United States, with more than 4 million of them, about 22%, being breast cancer survivors — a figure set to increase. We must recognize that this constitutes a significant patient population, and as a cancer center, we are excited to have a survivorship program to fully represent our patients.”
Transitioning from survivor to advocate
Mary Aalto, a patient advocate at the USC Norris cancer center, is one of those survivors. Celebrating her 19 years as a stage 3 breast cancer survivor, Aalto returned to the cancer center four years following her successful treatment — at the behest of her oncologist — to become a member of the center’s Cancer Survivorship Advisory Council. Shortly thereafter, she initiated an art series at the center’s cancer resource library showcasing the work of survivors, emphasizing resilience.
“Survivorship is receiving much attention now as individuals are living longer,” stated Aalto, whose mother succumbed to breast cancer during her childhood. “Decades ago, surviving stage 3 cancers was rare; doctors merely aimed to keep patients alive. Today, survivorship emphasizes quality of life, communication, and the doctor-patient rapport.”
Aalto also leads the center’s Patient Perspective Series, a year-round initiative featuring events where cancer survivors discuss pertinent topics, including clinical care, physician training, doctor-patient interactions, research, end-of-life regulations, and resilience. In her 11 years heading the program, she has hosted 66 events.
Aalto emphasizes part of her motivation to return as an advocate stemmed from the necessity for patient education and a greater comprehension of the significance of quality of life as patients, doctors, and other healthcare professionals develop care strategies.
“Despite rigorous treatment, my health is exceptional,” she reflected. “I experience gratitude every day, and I would not possess this level of appreciation had I not navigated through cancer. Interestingly, experiencing hardship allows one to treasure the good times.”
Where courage arises and hope flourishes
Uttam Sinha, director of the Head and Neck Center at Keck Medicine and a professor of otolaryngology — head and neck surgery at the Keck School of Medicine, pioneered a survivorship initiative for his department in the early 2000s.
“Cancer is rapidly evolving into a chronic condition; numerous patients are now living longer with cancer in remission,” Sinha noted, echoing Stewart’s assertion that society needs to learn how to properly care for and support cancer patients and their families.
He affirmed that survivorship programs are crucial for supplying patients with ongoing care and pertinent information throughout their journey — both during and after active treatment.
“There’s a wealth of information in cancer management, but retention rates are low as patients often feel overwhelmed,” Sinha observed. “I typically pair newly diagnosed patients with survivors who have navigated comparable experiences. This peer mentorship is invaluable.”
This mentorship approach holds particular significance when patients confront the physically and emotionally draining procedures commonly required in head and neck cancer treatment, such as tracheotomies (to facilitate breathing), mandibulectomies (removal of part or all of the jaw), or glossectomies (removal of part or all of the tongue).
“I comprehend the clinical process,” Sinha stated. “However, I have not experienced it firsthand. A survivor can convey an authentic perspective — what it feels like, how they managed, their healing journey. That’s a unique insight that only they can genuinely provide.”
The
“““html
The mission statement of the department’s survivorship initiative, “Where bravery is born and hope flourishes,” embodies a fundamental message that Sinha and his team advocate: inspiring patients to cherish life, discover empowerment within the community, and embrace their current circumstances, all while recognizing the grief and uncertainties that come with survivorship.
The program highlights four essential components of well-being: nutrition, stress management, physical activity, and sleep.
“The World Health Organization characterizes health as a comprehensive state of physical, mental, social, and spiritual well-being — not simply the absence of illness,” Sinha noted. “We often concentrate on physical recovery, yet the psychological and social dimensions are equally vital. Our survivorship programs aim to support those aspects thoroughly.”
Empowering patients for the journey
Before transitioning to physical therapy, Yamada worked as an orthopedic specialist and athletic trainer. Now, with two decades in oncology, she has been assisting patients in their recovery, helping them to improve more effectively and swiftly.
“I believe everyone has experienced a loved one, family member, or friend who has encountered cancer,” stated Yamada, whose grandfathers succumbed to cancer during her elementary school years.
She pointed out a widespread fallacy that life loses its meaning after cancer and that post-diagnosis quality of life is certain to diminish. “I want to emphasize that many of my earliest patients from that initial case load are still alive and flourishing,” she remarked.
Hope amid uncertainty
Duncan Wigg’s recovery starkly contradicts that fallacy. While he continues to receive immunotherapy for his initial lung cancer diagnosis, he characterizes his health as “excellent.” Just over a year ago, he was diagnosed with pancreatic cancer. After undergoing treatment, he encountered another challenging recovery phase but is anticipated to make a complete recuperation. He is actively engaged in intensive physical therapy with Yamada, receives consistent preventive care with his team of Keck Medicine professionals, and takes trips with his wife, a yoga instructor who, according to him, was also crucial to his recovery.
“I consider myself a bit of a miracle,” Wigg expressed. “But the healthcare system has advanced tremendously in research and knowledge over the last decade. I experienced only the finest cooperation among oncology, general surgery, radiology, and physical therapy — they were all communicating effectively.”
Mary Aalto shares Wigg’s optimistic outlook. “I am incredibly hopeful about the future for cancer survivors, because it continues to improve consistently,” she noted. “Individuals are living longer. They’re living healthier. They’re reclaiming the aspects of their lives that they cherished and thought they had lost when they were initially diagnosed.”
“`