Assessing the density of a cell can disclose a considerable amount regarding the cell’s condition. As cells multiply, specialize, or experience apoptosis, they may absorb or lose water and other substances, which becomes evident through alterations in density.
Monitoring these minute variations in the physical condition of cells on a large scale can be quite challenging, particularly with single-cell precision, but a research team at MIT has discovered a method to assess cell density swiftly and precisely — evaluating up to 30,000 cells in just one hour.
The researchers demonstrated that alterations in density could be leveraged to make significant predictions, such as whether immune cells like T cells have been activated to target tumors, or if tumor cells are vulnerable to a specific medication.
“These predictions are all derived from observing very minor shifts in the physical characteristics of cells, which can indicate how they will react,” explains Scott Manalis, the David H. Koch Professor of Engineering in the Biological Engineering and Mechanical Engineering departments, and a member of the Koch Institute for Integrative Cancer Research.
Manalis serves as the senior author of the recent study, which is published today in Nature Biomedical Engineering. The lead author of the paper is MIT Research Scientist Weida (Richard) Wu.
Assessing density
As cells transition into new states, their molecular composition, including lipids, proteins, and nucleic acids, may become more or less congested. Evaluating the density of a cell provides an indirect perspective on this congestion.
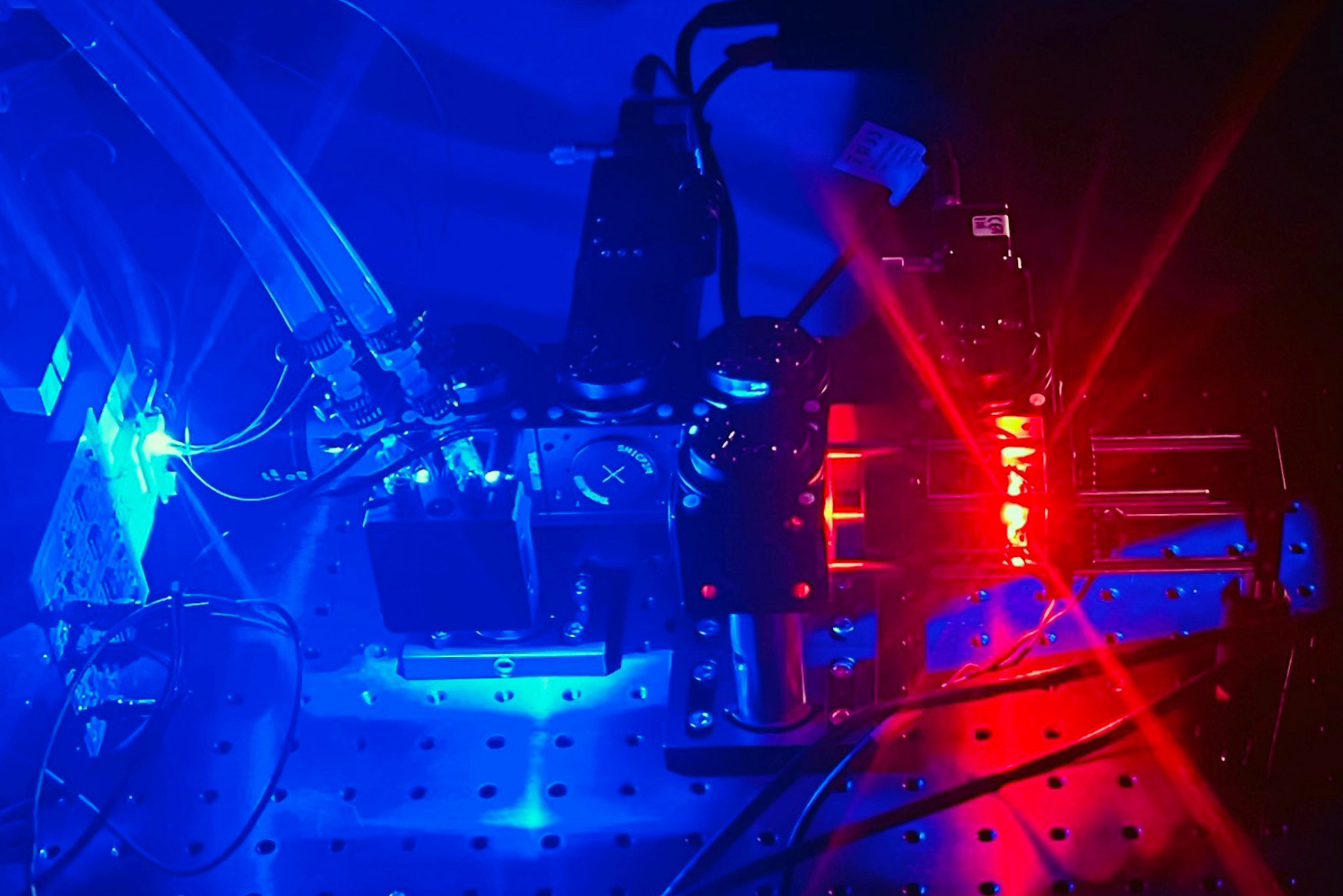
The novel density measurement technique detailed in this research builds upon the work that Manalis’ lab has conducted over the last twenty years on technologies for measuring cells and minuscule particles. In 2007, his lab created a microfluidic apparatus called a suspended microchannel resonator (SMR), comprising a microchannel across a small silicon cantilever that vibrates at a defined frequency. When a cell moves through the channel, the vibration frequency alters slightly, and the extent of that change can be utilized to compute the cell’s mass.
In 2011, the researchers modified the technique to assess cell density. To accomplish this, cells are directed through the device twice, suspended in two different liquid densities. A cell’s buoyant mass (its mass while floating in fluid) is influenced by its total mass and volume; therefore, by measuring two distinct buoyant masses for a cell, its mass, volume, and density can be computed.
This method is effective, but changing fluids and passing cells through each one is labor-intensive, limiting its application to measuring only a few hundred cells at once.
To devise a quicker, more efficient system, the researchers integrated their SMR device with a fluorescent microscope tailored for cell volume measurements. The microscope is located at the entrance to the resonator, and cells flow through the apparatus while suspended in a fluorescent dye that is not absorbed by the cells. When cells pass the microscope, the reduction in the fluorescent signal can be used to determine the cell’s volume.
Once the volume measurement is completed, the cells enter the resonator, which gauges their mass. This approach permits rapid density calculations and can assess up to 30,000 cells in an hour.
“Rather than having the cells move back and forth through the cantilever multiple times to determine cell density, we aimed to establish a method for streamlined measurement, enabling cells to pass through the cantilever just once,” Wu states. “From a cell’s mass and volume, we can then derive its density, maintaining both throughput and accuracy.”
Assessing T cells
The researchers employed their new method to monitor changes in the density of T cells following their activation by signaling molecules.
As T cells shift from a dormant state to an active one, they acquire new molecules and water, as the researchers discovered. From their pre-activation condition to the first day of activation, the cells’ densities decreased from an average of 1.08 grams per milliliter to 1.06 grams per milliliter. This indicates that the cells are becoming less crowded, as they absorb water more rapidly than they accumulate other substances.
“This suggests that cell density likely corresponds to an increase in cellular water content as the cells transition from a dormant, non-proliferative phase to a high-growth phase,” Wu notes. “These findings indicate that cell density is an intriguing biomarker that changes during T-cell activation and may have functional relevance concerning how effectively the T cells can proliferate.”
Travera, a clinical-stage enterprise co-founded by Manalis, is exploring the use of SMR mass measurements to anticipate whether individual cancer patients’ T cells will respond to drugs designed to elicit a robust anti-tumor immune reaction. The company has also initiated the application of the density measurement method, and preliminary studies have revealed that combining mass and density measurements yields a far more precise prediction than using either metric individually.
“Both mass and density unveil significant insights about the overall capability of the immune cells,” Manalis remarks.
Utilizing physical measurements of cells to track their immune activation “is truly exciting and could provide a novel method for assessing and monitoring modifications in immune cells circulating in the body,” remarks Genevieve Boland, an associate professor of surgery at Harvard Medical School and vice chair of research for the Integrated Department of Surgery at Mass General Brigham, who was not associated with the study.
“This represents a complementary but distinct approach compared to current methods used for immune evaluations in cancer and other diseases, potentially supplying a groundbreaking tool to aid in clinical decision-making regarding the necessity for and selection of specific cancer treatments, enable monitoring of therapy responses, and/or facilitate the early identification of side effects from immunotherapy,” she states.
Making predictions
Another potential application for this technique is forecasting how tumor cells might react to various cancer drugs. In prior research, Manalis demonstrated that monitoring changes in cell mass post-treatment could predict whether a tumor cell is experiencing drug-induced apoptosis. In the new investigation, he discovered that density changes could also indicate these responses.
In these experiments, the researchers treated pancreatic cancer cells with two distinct drugs — one that the cells can be sensitive to, and another to which they are resistant. They found that variations in density post-treatment accurately mirrored the cells’ known reactions to the treatments.
“We capture essential information about the cells that is highly predictive within the initial few days after their removal from the tumor,” Wu indicates. “Cell density serves as a rapid biomarker to predict in vivo drug response in a timely fashion.”
Manalis’ lab is now focusing on utilizing measurements of cell mass and density to assess the viability of cells employed in the synthesis of complex proteins like therapeutic antibodies.
“As cells fabricate these proteins, we can glean insights from these markers of cell viability and metabolic condition to make predictions about how well these cells can produce these proteins, and ideally, in the future, also direct design and control strategies to further optimize the yield of these intricate proteins,” Wu explains.
The research was supported by the Paul G. Allen Frontiers Group, the Virginia and Daniel K. Ludwig Fund for Cancer Research, the MIT Center for Precision Cancer Medicine, the Stand Up to Cancer Convergence Program, Bristol Myers Squibb, and the Koch Institute Support (core) Grant from the National Cancer Institute.