Investigators at MIT and the Scripps Research Institute have demonstrated that they can elicit a robust immune response to HIV with merely a single vaccine dose, by incorporating two potent adjuvants — substances that enhance immune system activation.
In a study involving mice, the investigators found that this method yielded a considerably broader spectrum of antibodies against an HIV antigen, in contrast to the vaccine administered alone or combined with just one of the adjuvants. The dual-adjuvant vaccine accumulated in the lymph nodes and persisted there for up to a month, enabling the immune system to develop a significantly larger quantity of antibodies against the HIV protein.
This technique may pave the way for vaccines that require only one administration for infectious illnesses, including HIV or SARS-CoV-2, according to the researchers.
“This method is amenable to various protein-based vaccines, offering the potential to formulate new preparations for these vaccine types across a wide array of diseases, including influenza, SARS-CoV-2, or other pandemic situations,” states J. Christopher Love, the Raymond A. and Helen E. St. Laurent Professor of Chemical Engineering at MIT and a member of the Koch Institute for Integrative Cancer Research and the Ragon Institute of MGH, MIT, and Harvard.
Love and Darrell Irvine, a professor of immunology and microbiology at the Scripps Research Institute, are the lead authors of the study, which is published today in Science Translational Medicine. Kristen Rodrigues PhD ’23 and Yiming Zhang PhD ’25 are the lead authors of the manuscript.
Stronger Vaccines
Most vaccines are administered together with adjuvants that contribute to a more vigorous immune response to the antigen. A frequently used adjuvant alongside protein-based vaccines, like those for hepatitis A and B, is aluminum hydroxide, commonly referred to as alum. This adjuvant functions by activating the innate immune response, aiding the body in forming a more robust memory of the vaccine antigen.
A few years ago, Irvine developed another adjuvant based on saponin, an FDA-approved adjuvant sourced from the bark of the Chilean soapbark tree. His research indicated that nanoparticles containing both saponin and a molecule called MPLA, which stimulates inflammation, were more effective than saponin alone. This nanoparticle, known as SMNP, is currently being utilized as an adjuvant for an HIV vaccine that is undergoing clinical trials.
Irvine and Love subsequently experimented with combining alum and SMNP, demonstrating that vaccines incorporating both adjuvants could elicit even stronger immune responses against either HIV or SARS-CoV-2.
In their latest paper, the researchers aimed to investigate why these two adjuvants function so effectively in tandem to enhance the immune response, particularly the B cell response. B cells produce antibodies capable of circulating in the bloodstream and recognizing a pathogen if re-exposed.
For this investigation, the scientists utilized an HIV protein named MD39 as their vaccine antigen, anchoring numerous of these proteins to each alum particle, along with SMNP.
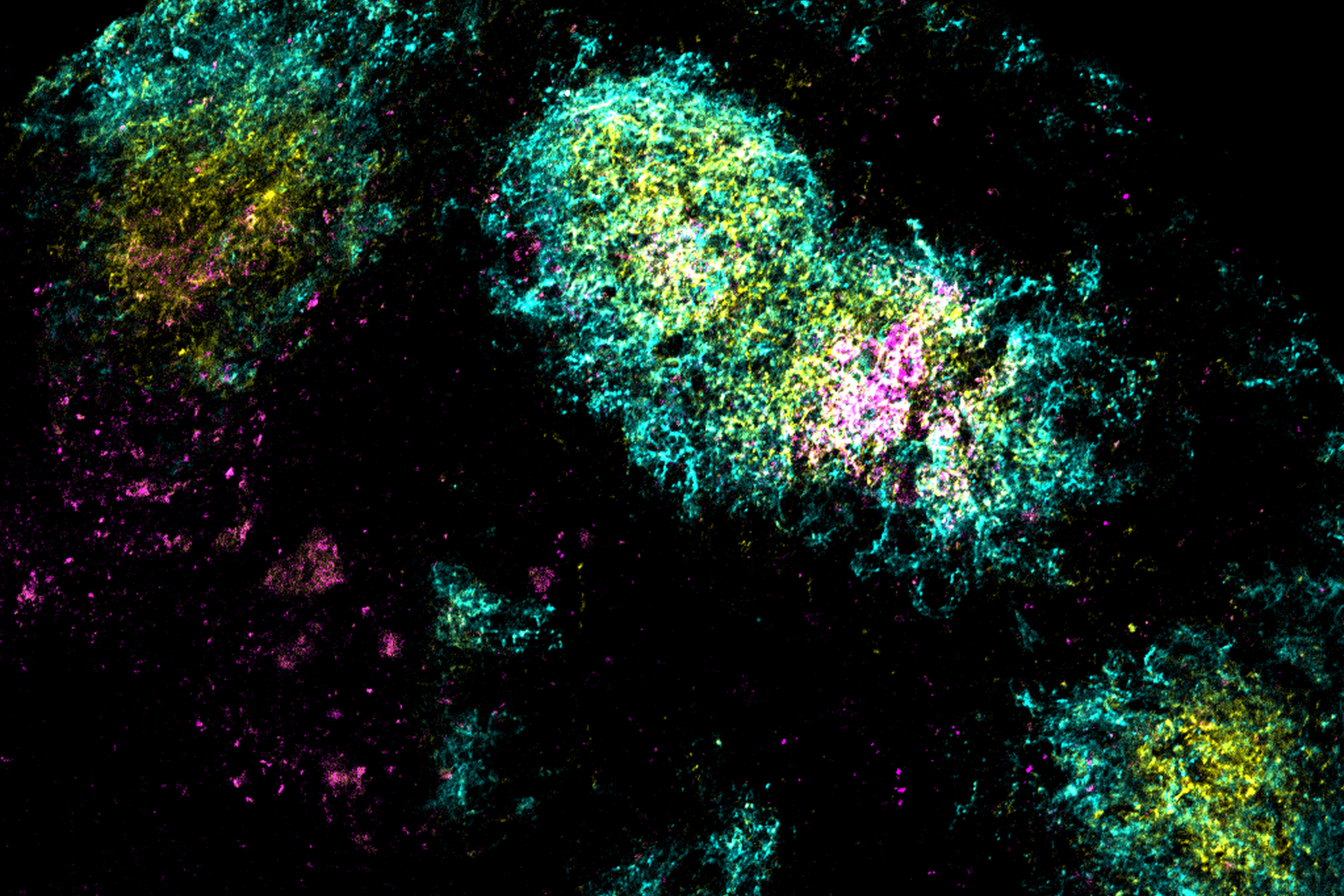
Following the vaccination of mice with these particles, the researchers discovered that the vaccine accumulated in the lymph nodes — areas where B cells encounter antigens and undergo rapid mutations that generate antibodies with high affinity to a specific antigen. This process occurs within clusters of cells referred to as germinal centers.
The researchers demonstrated that SMNP and alum assisted the HIV antigen in penetrating the protective barrier of cells surrounding the lymph nodes without breaking down into smaller fragments. The adjuvants also ensured that the antigens remained intact in the lymph nodes for up to 28 days.
“Consequently, the B cells cycling in the lymph nodes are consistently exposed to the antigen throughout this period, allowing them to refine their approach to the antigen,” Love says.
This strategy may replicate what happens during a natural infection, where antigens can stay in the lymph nodes for weeks, giving the body time to mount an immune response.
Antibody Diversity
Single-cell RNA sequencing of B cells from the vaccinated mice revealed that the vaccine containing both adjuvants produced a far more diverse collection of B cells and antibodies. Mice that received the dual-adjuvant vaccine had two to three times more unique B cells than those that were given only one of the adjuvants.
This increase in B cell quantity and diversity enhances the likelihood that the vaccine could generate broadly neutralizing antibodies — antibodies capable of recognizing a variety of virus strains, such as HIV.
“When considering the immune system sampling all possible solutions, the more opportunities we provide it to find an effective solution, the better,” Love explains. “Generating broadly neutralizing antibodies is likely something that requires both the kind of method we demonstrated here, to achieve that strong and diversified response, as well as careful antigen design to highlight the correct part of the immunogen.”
Utilizing these two adjuvants together may also aid in the creation of more potent vaccines against various infectious diseases, requiring just a single administration.
“What’s potentially remarkable about this method is that it allows for extended exposure based on a combination of adjuvants that are already well-understood, eliminating the need for new technologies. It simply combines features of these adjuvants to enable low-dose or possibly even single-dose treatments,” Love remarks.
The research received funding from the National Institutes of Health; the Koch Institute Support (core) Grant from the National Cancer Institute; the Ragon Institute of MGH, MIT, and Harvard; and the Howard Hughes Medical Institute.