“`html
The most prevalent form of brain tumor in youngsters, pilocytic astrocytoma (PA), constitutes approximately 15% of all pediatric brain neoplasms. While this type of tumor is generally not fatal, uncontrolled proliferation of tumor cells can interfere with normal brain development and functionality. Present therapies predominantly target the excision of tumor cells, yet recent research indicates that non-cancerous cells, like nerve cells, also contribute to the development and proliferation of brain tumors, opening avenues for innovative treatment methods.
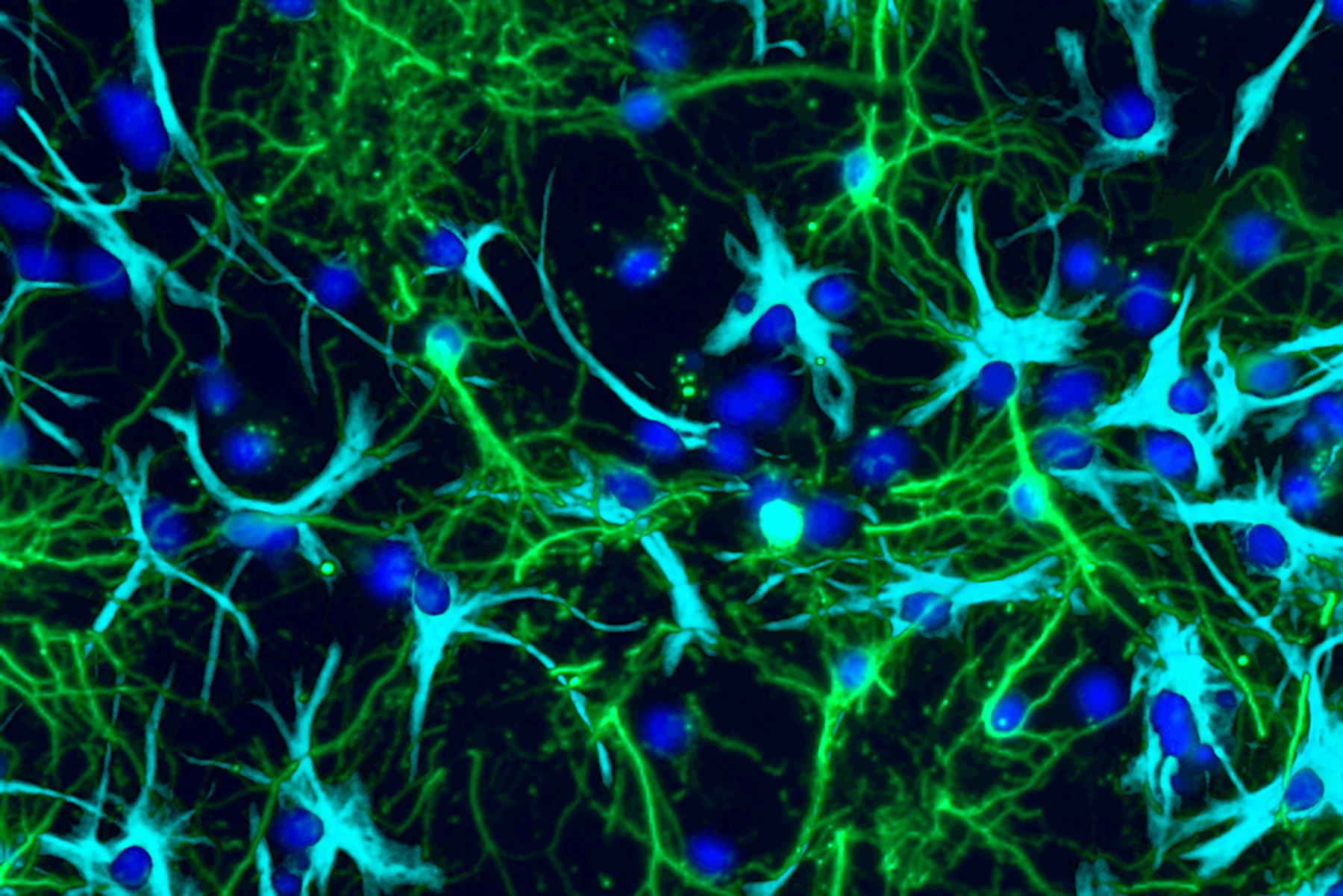
Researchers have long recognized that a nerve cell signaling substance known as glutamate can promote cancer growth throughout the body. However, after extensive study, they have yet to definitively determine the mechanism behind this process or how to inhibit it. Now, a multidisciplinary group of investigators at Washington University School of Medicine in St. Louis has revealed how glutamate influences the growth of pediatric brain tumors. Utilizing tumor cells obtained from patient PA samples, they found that PA cells commandeer the function of proteins on cellular surfaces that typically respond to glutamate, termed glutamate receptors. Rather than conveying glutamate’s standard electrical signal, these receptors are reprogrammed to emit signals that enhance cellular growth.
Additionally, the team observed that medications which inhibit these glutamate receptors—such as memantine, approved for the treatment of dementia and Alzheimer’s disease—decreased the growth of human pediatric brain tumors in mice, indicating a promising new therapeutic possibility.
The findings are set to be published on Sept. 1 in Neuron.
“With respect to these kinds of pediatric brain tumors, our arsenal for treating patients is quite limited,” stated senior author David Gutmann, MD, PhD, the Donald O. Schnuck Family Professor of Neurology at WashU Medicine. Gutmann provides care for patients at Siteman Kids at St. Louis Children’s Hospital. “The prospect of repurposing drugs already utilized for various neurological disorders suggests we might have additional strategies available for patient treatment.”
The research group, which featured first author Corina Anastasaki, PhD, a research assistant professor of neurology at WashU Medicine, also demonstrated for the first time that glutamate receptors incorrectly associate with growth receptors in PAs, thereby fueling the tumors. These insights provide a blueprint for future investigations into whether similar mechanisms are at play in other cancer types.
Reinventing familiar instruments
Glutamate is classified as a neurotransmitter, a molecule enabling communication among nerve cells, including neurons in the brain. In their endeavor to unravel how glutamate promotes brain tumor growth, Gutmann—who is also the director of the Neurofibromatosis Center at WashU Medicine—and Anastasaki collaborated with colleagues across various disciplines within WashU Medicine—such as neurosurgery, pediatrics, genetics, neuropathology, biostatistics, and beyond—to gather and analyze surgically removed PA samples. They discovered that these PA cells exhibited abnormally elevated levels of glutamate receptors.
Through testing the influence of glutamate on these tumors, the researchers determined that glutamate heightened PA cell populations by initiating a cascade of reactions within the tumor cells that encouraged cellular division. These findings imply that tumor cells utilize typical interactions between brain cells to accelerate their own growth.
“This innovative mechanism for tumor proliferation merges two ordinary yet disconnected brain processes—growth and electrical signaling—in an irregular manner,” Anastasaki remarked. “Now that we’ve deciphered how these cells operate and proliferate, the possibilities are endless for investigating other neurotransmitters and the diverse communication pathways between neurons and cancer cells. Comprehending this will clarify why tumors develop and behave as they do, potentially leading to significantly different treatment approaches.”
Such innovative therapies may arise from well-known sources. The researchers indicated that the inhibition of glutamate receptors in tumor cells in mice with PAs—either via pharmaceuticals or genetic modifications—reduced tumor size. This highlights a potential opportunity to repurpose drugs targeting glutamate receptors, such as memantine, for PA treatment.
The next stages involve determining the safety of such medications for pediatric patients with brain tumors and the appropriate dosages for effectiveness, as noted by Gutmann, which will necessitate clinical trials.
“This investigation provides compelling preclinical evidence to consider medications that are otherwise safe and authorized for treating other neurological disorders,” Gutmann said. “This could pave the way for new therapeutic strategies and help minimize the impact on a child’s developing brain by decreasing interactions between brain cells and tumor cells.”
Anastasaki C, Mu R, Kernan CM, Li X, Barakat R, Koleske JP, Gao Y, Cobb OM, Lu X, Eberhart CG, Phillips JJ, Strahle JM, Dahiya S, Mennerick SJ, Rodriguez FJ, Gutmann D. Aberrant coupling of glutamate and tyrosine kinase receptors enables neuronal control of brain tumor growth. Neuron. September 1, 2025.
This research was partially supported by grants from the National Institute of Neurological Disorders and Stroke (R35NS07211-01), National Cancer Institute (1-R50-CA233164-01), National Institutes of Health (P50MH122379 and R01MH123748), Taylor Family Institute for Innovative Psychiatric Research, and the Pediatric Brain Tumor Foundation. Corrine Gardner and the Pediatric Neurosurgery Tissue Bank facilitated the procurement of fresh surgical samples. The content is solely the authors’ responsibility and does not necessarily represent the official views of the NIH.
About Washington University School of Medicine
WashU Medicine is a global frontrunner in academic medicine, encompassing biomedical research, patient care, and educational programs with 2,900 faculty members. Its National Institutes of Health (NIH) research funding portfolio ranks second among U.S. medical schools and has increased by 83% since 2016. In conjunction with institutional investments, WashU Medicine allocates well over $1 billion annually to fundamental and clinical research innovation and training. Its faculty practice consistently ranks among the top five nationally, with over 1,900 faculty physicians delivering care at 130 locations. WashU Medicine’s physicians exclusively staff Barnes-Jewish and St. Louis Children’s hospitals—the academic hospitals of BJC HealthCare—and care for patients at BJC’s community hospitals in the region. WashU Medicine has a rich history in MD/PhD training, recently committed $100 million to scholarships and curriculum renewal for its medical students, and hosts exceptional training programs in every medical subspecialty, including physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website
The post Study sheds light on how pediatric brain tumors grow appeared first on The Source.
“`