“`html
A recent investigation by MIT neuroscientists uncovers how uncommon variants of a gene known as ABCA7 may influence the onset of Alzheimer’s in certain individuals who possess it.
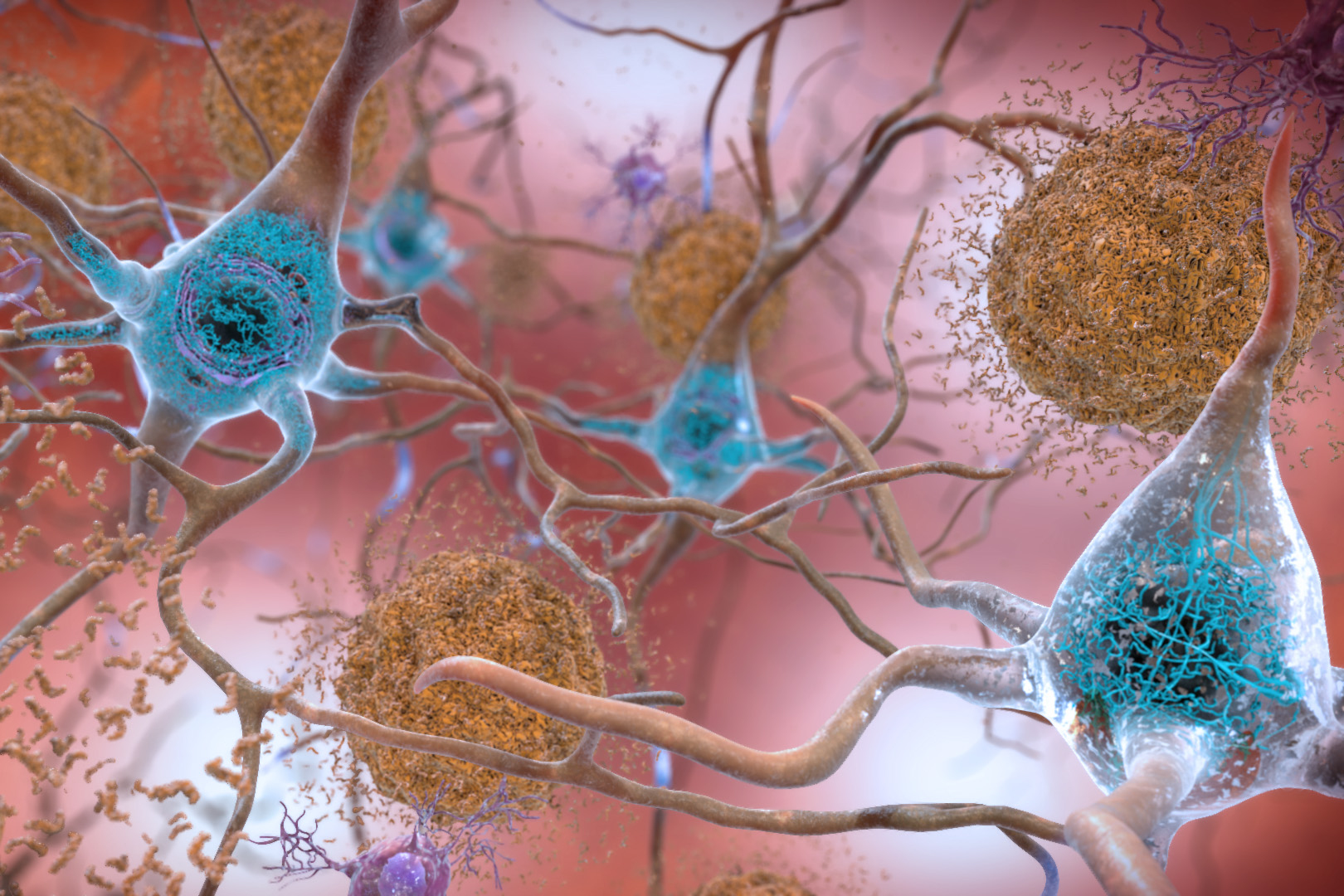
Malfunctioning versions of the ABCA7 gene, which exist in a very small segment of the population, significantly heighten the risk of Alzheimer’s. In the latest research, the scientists found that these mutations can interfere with the metabolism of lipids essential for cell membranes.
This interference causes neurons to become excessively excitable, plunging them into a stressed condition that may harm DNA and other cellular elements. The researchers discovered that these outcomes could potentially be countered by administering choline, a crucial precursor necessary for the formation of cell membranes.
“We observed quite strikingly that when we treated these cells with choline, many of the transcriptional anomalies were restored. We also noted that the hyperexcitability characteristic and increased levels of amyloid beta peptides observed in neurons lacking ABCA7 were diminished post-treatment,” states Djuna von Maydell, an MIT graduate student and the principal author of the research.
Li-Huei Tsai, director of MIT’s Picower Institute for Learning and Memory and the Picower Professor in the MIT Department of Brain and Cognitive Sciences, is the senior author of the article, published today in Nature.
Membrane impairment
Genomic research involving Alzheimer’s patients has indicated that individuals with variants of ABCA7 that result in diminished levels of functional ABCA7 protein are approximately twice as likely to develop Alzheimer’s as those without these variants.
ABCA7 codes for a protein that facilitates the transport of lipids across cell membranes. Lipid metabolism is also a primary focus of a more prevalent Alzheimer’s risk factor known as APOE4. In prior research, Tsai’s lab has demonstrated that APOE4, found in about half of all Alzheimer’s patients, disrupts the ability of brain cells to metabolize lipids and respond to stress.
To investigate how ABCA7 variants might elevate Alzheimer’s risk, the researchers obtained tissue samples from the Religious Orders Study/Memory and Aging Project (ROSMAP), a long-term study monitoring memory, motor, and other age-related transformations in older adults since 1994. Of roughly 1,200 samples in the dataset with available genetic information, the researchers acquired 12 from individuals carrying a rare ABCA7 variant.
The researchers executed single-cell RNA sequencing of neurons from these ABCA7 carriers, enabling them to ascertain which other genes are influenced when ABCA7 is absent. They discovered that the most significantly impacted genes fell into three categories associated with lipid metabolism, DNA damage, and oxidative phosphorylation (the metabolic mechanism that cells utilize to harness energy as ATP).
To delve into how these changes could impact neuronal function, the researchers introduced ABCA7 variants into neurons derived from induced pluripotent stem cells.
These cells exhibited numerous gene expression alterations similar to those from patient samples, particularly among genes related to oxidative phosphorylation. Additional experiments indicated that the “safety valve” typically allowing mitochondria to limit excessive electrical charge build-up was less active. This scenario can lead to oxidative stress, a condition occurring when an excess of cell-damaging free radicals accumulates in tissues.
Using these modified cells, the researchers also examined the consequences of ABCA7 variants on lipid metabolism. Cells with the variants modified the metabolism of a molecule called phosphatidylcholine, potentially resulting in membrane rigidity and possibly elucidating why the mitochondrial membranes of the cells could not function normally.
An increase in choline
These discoveries raised the potential that intervening in phosphatidylcholine metabolism could reverse some of the cellular implications of ABCA7 loss. To evaluate this notion, the researchers treated neurons with ABCA7 mutations using a molecule named CDP-choline, a precursor of phosphatidylcholine.
As these cells initiated the production of new phosphatidylcholine (both saturated and unsaturated forms), their mitochondrial membrane potentials normalized, and oxidative stress levels decreased.
The researchers then utilized induced pluripotent stem cells to create 3D tissue organoids composed of neurons with the ABCA7 variant. These organoids exhibited elevated levels of amyloid beta proteins, which constitute the plaques observed in the brains of Alzheimer’s patients. However, those levels reverted to normal when the organoids were treated with CDP-choline. The treatment also mitigated the hyperexcitability in neurons.
In a 2021 publication, Tsai’s lab found that CDP-choline treatment could similarly reverse many effects of another Alzheimer’s-associated gene variant, APOE4, in mice. She is currently collaborating with researchers at the University of Texas and MD Anderson Cancer Center on a clinical trial examining how choline supplements influence individuals carrying the APOE4 gene.
Choline is naturally present in foods such as eggs, meat, fish, and some legumes and nuts. Enhancing choline intake with supplements may provide a method for many to lower their risk of Alzheimer’s disease, Tsai states.
“From APOE4 to ABCA7 loss of function, my lab illustrates that disruption of lipid homeostasis leads to the emergence of Alzheimer’s-related pathology, and that reinstating lipid homeostasis, such as through choline supplementation, can improve these pathological traits,” she asserts.
Alongside the rare variants of ABCA7 studied in this research, there exists a more prevalent variant found at a frequency of around 18 percent in the population. This variant was previously believed to be innocuous, but the MIT team demonstrated that cells with this variant showed numerous similar gene changes in lipid metabolism as seen in cells with the rare ABCA7 variants.
“There’s still more research needed in this area, but this suggests that ABCA7 dysfunction could significantly impact a larger segment of the population beyond just those carrying the rare variants,” von Maydell notes.
The investigation was partially funded by the Cure Alzheimer’s Fund, the Freedom Together Foundation, the Carol and Gene Ludwig Family Foundation, James D. Cook, and the National Institutes of Health.
“`