A recent investigation from Washington University School of Medicine in St. Louis uncovers a potential method to decelerate or halt the advancement of age-related macular degeneration, a primary contributor to blindness in individuals over 50 years old. Researchers at WashU Medicine, alongside their global partners, indicated that issues with cholesterol processing may be linked to this form of vision impairment, possibly shedding light on the connections between macular degeneration and cardiovascular conditions, both of which deteriorate with age.
The novel insights — discovered through human plasma samples and murine models of macular degeneration — propose that augmenting the concentration of a molecule known as apolipoprotein M (ApoM) in the bloodstream addresses deficiencies in cholesterol management that result in cellular harm in the eyes and other bodily organs. Diverse strategies for enhancing ApoM levels could emerge as innovative treatment options for age-related macular degeneration and potentially for certain types of heart failure induced by similar cholesterol metabolism dysfunctions.
This research was published on June 24 in the journal Nature Communications.
“Our investigation highlights a potential pathway to meet a significant unmet clinical demand,” stated senior author Rajendra S. Apte, MD, PhD, the Paul A. Cibis Distinguished Professor of Ophthalmology and Visual Sciences at WashU Medicine. “Existing therapies that diminish the risk of additional vision impairment are restricted to only the most severe phases of macular degeneration and do not reverse the condition. Our results imply that creating interventions that elevate ApoM levels could effectively treat or even avert the disease, hence safeguarding individuals’ eyesight as they age.”
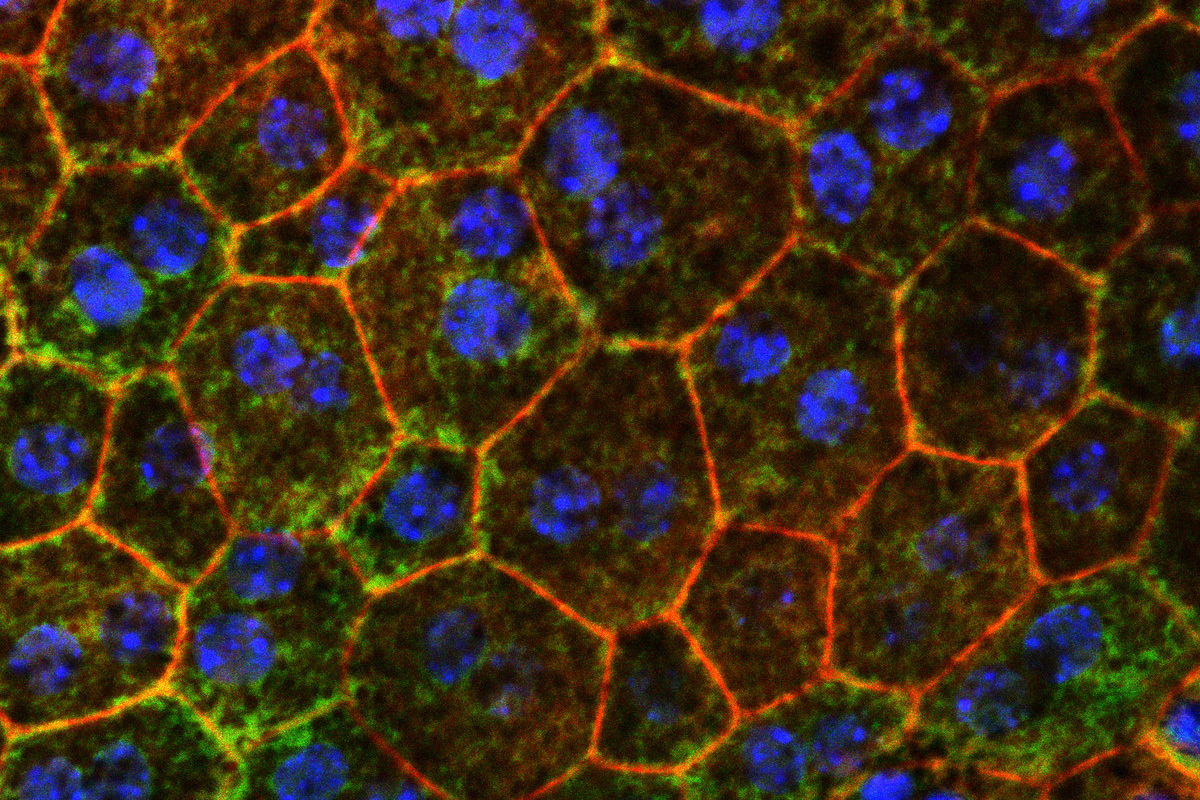
In cases of macular degeneration, clinicians can observe cholesterol-laden deposits beneath the retina during an ocular examination, according to Apte. In preliminary stages, vision may appear unaffected, yet the deposits heighten inflammation and other detrimental processes that contribute to a gradual loss of central vision. In the most prevalent form, “dry” macular degeneration, the cells in the central retina may suffer damage, leading to a neurodegenerative condition known as geographic atrophy, similar to the processes seen in the brain during ailments such as Alzheimer’s disease. Dry macular degeneration can progress to “wet” macular degeneration, characterized by abnormal vascular proliferation that impairs vision.
Geographic atrophy and wet macular degeneration represent advanced stages of the disease that are associated with visual impairment. While some approved therapies for advanced disease exist, the disease’s progress at that point is irreversible.
A common instigator in ocular disease and heart failure
In recent years, data have surfaced indicating that ApoM can function as a protective agent with established anti-inflammatory properties and roles in sustaining proper cholesterol metabolism. Given this context, Apte and co-senior author Ali Javaheri, MD, PhD, an assistant professor of medicine, sought to investigate whether diminished ApoM levels, which decline with age, could contribute to the impaired cholesterol metabolism underlying various age-related diseases, including macular degeneration and heart disease. They demonstrated that individuals with macular degeneration exhibit lower levels of ApoM circulating in the bloodstream when compared to healthy subjects. Additionally, prior research by Javaheri, a WashU Medicine cardiologist, established that patients experiencing different types of heart failure also had decreased ApoM levels in their bloodstream.
This study highlighted that ApoM is a crucial element in the “good cholesterol” pathways responsible for clearing excess harmful cholesterol — known to exacerbate inflammation — from the body via the liver.
Apte and Javaheri’s findings suggest that when ApoM levels are low, cells within the retina and heart tissue struggle to properly process cholesterol deposits and face challenges in eliminating these accumulating lipids. As these lipids accumulate, they lead to inflammation and cellular damage.
To ascertain whether they could counteract the negative impacts of low ApoM, the researchers elevated ApoM levels in murine models of macular degeneration, utilizing genetic modification or plasma transfer from other mice. The mice exhibited signs of enhanced retinal health, improved function of light-sensitive cells in the retina, and less cholesterol deposit accumulation. Furthermore, the researchers identified that ApoM activates a signaling pathway that facilitates the breakdown of cholesterol within cellular structures known as lysosomes, recognized for their vital role in managing cellular waste.
The investigation also indicated that ApoM must be associated with a molecule named sphingosine-1-phosphate (S1P) to realize the advantageous effects of ApoM treatment in the mice.
Apte and Javaheri are collaborating with Mobius Scientific, a WashU startup focused on leveraging this understanding of ApoM’s role in macular degeneration to formulate new methodologies for treating or preventing the condition. In 2022, Apte and Javaheri teamed with WashU’s Office of Technology Management to establish Mobius Scientific.
The results could also hold promise for future strategies aimed at elevating ApoM in patients experiencing heart failure.
“One of the thrilling aspects of this collaboration is recognizing the connections between retinal pigment epithelial cells and cardiac muscle cells, both of which are susceptible to low ApoM,” Javaheri remarked. “There is a possibility that the interaction between ApoM and S1P is influencing cholesterol metabolism in both cell types. We eagerly anticipate investigating strategies to enhance ApoM in ways that might assist the eye and heart in maintaining healthy cholesterol metabolism over time and counteract two significant aging-related diseases.”
Lee TJ, Santeford A, Pitts KM, Valenzuela Ripoll C, Terao R, Guo Z, Ozcan M, Kratky D, Christoffersen C, Javaheri A, Apte RS. Apolipoprotein M mitigates age-related macular degeneration characteristics via sphingosine-1-phosphate signaling and lysosomal lipid degradation. Nature Communications. June 24, 2025. DOI: 10.1038/s41467-025-60830-1
This research was funded by the National Institutes of Health (NIH), grant numbers R01 EY019287, P30 EY02687, 1T32GM1397740-1, K08HL138262, 1R01HL155344, P30DK020579, and P30DK056341; the Jeffrey T. Fort Innovation Fund; the Starr Foundation AMD Research Fund; the Siteman Retina Research Fund; a Research to Prevent Blindness/American Macular Degeneration Foundation Catalyst Award for Innovative Research Approaches for Age-Related Macular Degeneration; the Carl Marshall and Mildred Almen Reeves Foundation; the Retina Associates of St. Louis Research Fund; a pilot project grant from the Washington University Genome Technology Access Center; an unrestricted grant from Research to Prevent Blindness to the John F. Hardesty, MD Department of Ophthalmology and Visual Sciences at Washington University School of Medicine in St. Louis; a Vitreoretinal Surgery Foundation Fellowship, number VGR0023118; the Children’s Discovery Institute of Washington University and St. Louis Children’s Hospital, grant number MC-FR-2020-919; the Longer Life Foundation; and by the Austrian Science Fund, grant number SFB 10.55776/F73.
The content solely reflects the views of the authors and does not necessarily represent the official perspectives of the NIH.
Apte and Javaheri have intellectual property applications licensed by Washington University to Mobius Scientific. Apte currently serves as the chief scientific officer at Mobius Scientific, and both members are part of the advisory board for the company.
About Washington University School of Medicine
WashU Medicine is a prominent institution in academic medicine, covering biomedical research, patient care, and educational programs with 2,900 faculty members. Its National Institutes of Health (NIH) research funding portfolio ranks second among U.S. medical schools and has increased by 83% since 2016. Alongside institutional investment, WashU Medicine allocates over $1 billion annually to basic and clinical research innovations and education. Its faculty practice consistently ranks among the top five nationally, featuring over 1,900 faculty physicians practicing across 130 locations, who also comprise the medical staff at Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine boasts a distinguished history in MD/PhD training, having recently dedicated $100 million to scholarship funding and curriculum enhancement for its medical students, and hosts premier training programs in every medical subspecialty, as well as in physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website
The post Strategy to prevent age-related macular degeneration identified appeared first on The Source.