“`html
Science & Tech
Planting ideas for bipolar disorder
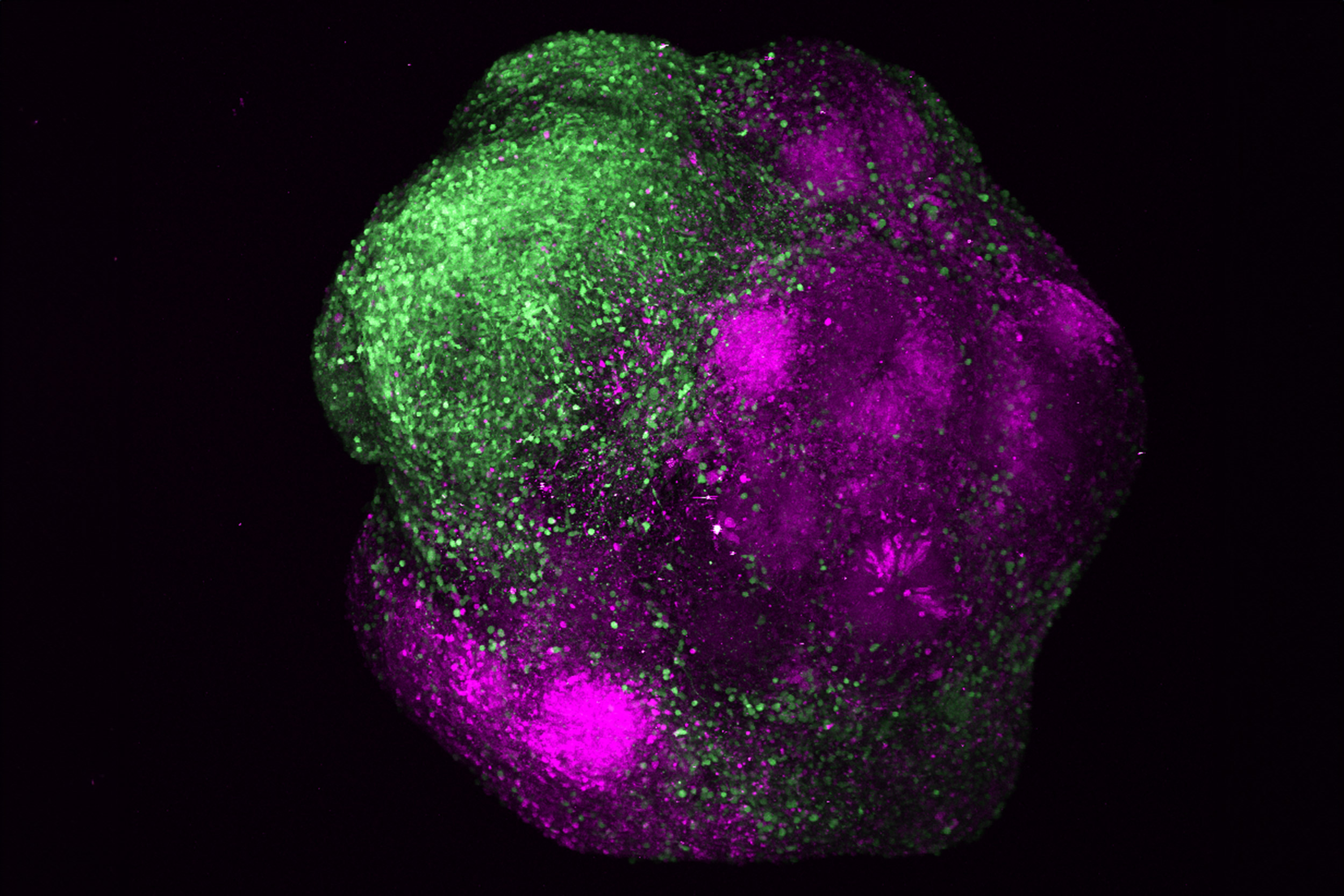
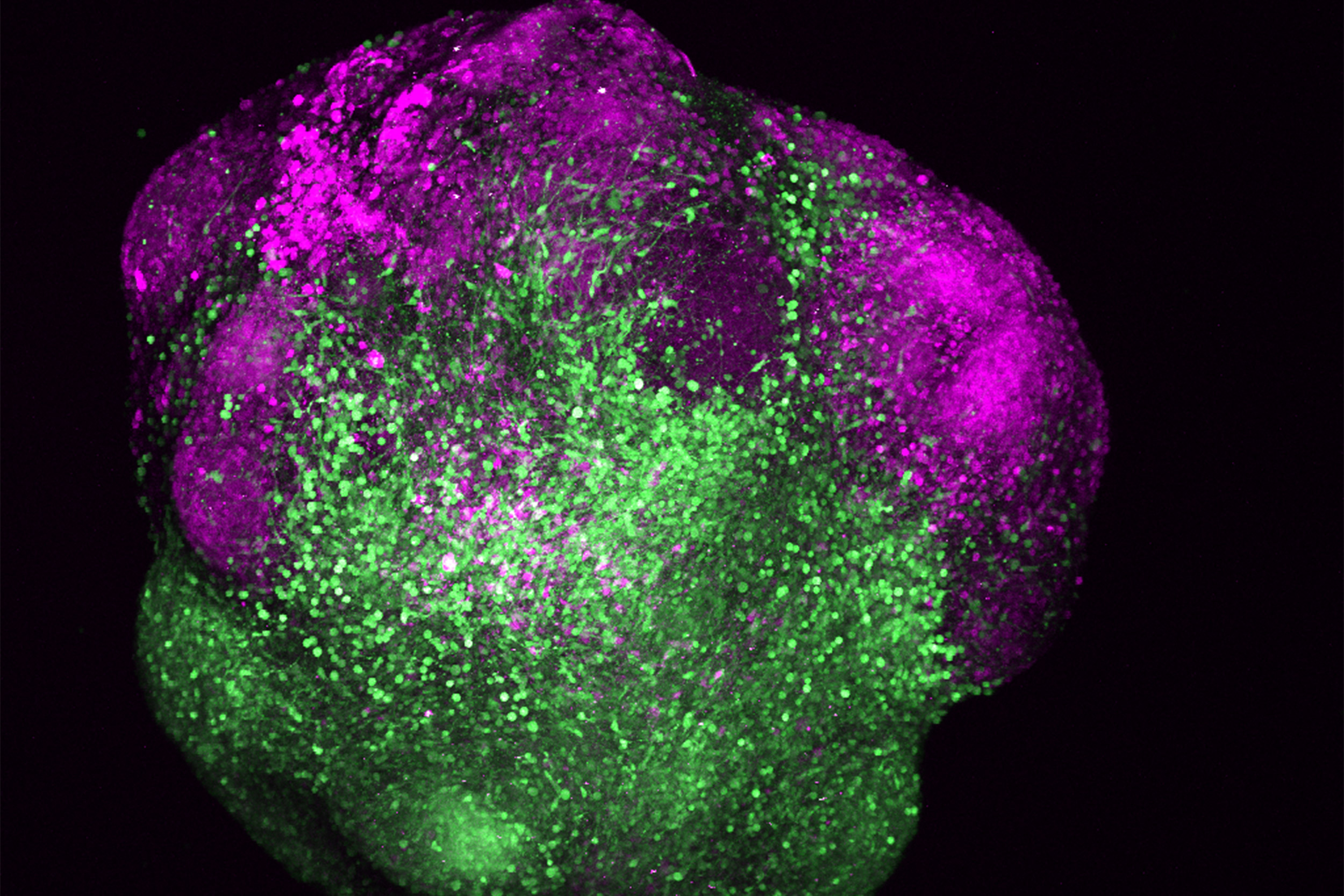
Human brain organoid displaying the integration of excitatory (magenta) and inhibitory neurons (green) of the cerebral cortex.
Credit: Arlotta Lab
Brain Science grants encourage fresh methods to tackle the condition and uncover underlying factors
Paola Arlotta lifts a vial filled with clear liquid swirling with tiny spheres. When she shakes her wrist, the shapes dance like elements within a snow globe.
“Those tiny orbs swirling around are actually small segments of human cerebral cortex,” stated Arlotta, the Golub Family Professor of Stem Cell and Regenerative Biology, “except instead of originating from the brain of an individual, they were cultivated in the laboratory.”
These diminutive shapes may signify a significant opportunity for advances in understanding bipolar disorder, a mental health issue impacting approximately 8 million individuals in the U.S. These lab-created “organoids” — brain-like tissue synthesized from blood cells of living patients — provide a pathway to discover more effective medications and create more individualized treatments for bipolar patients.
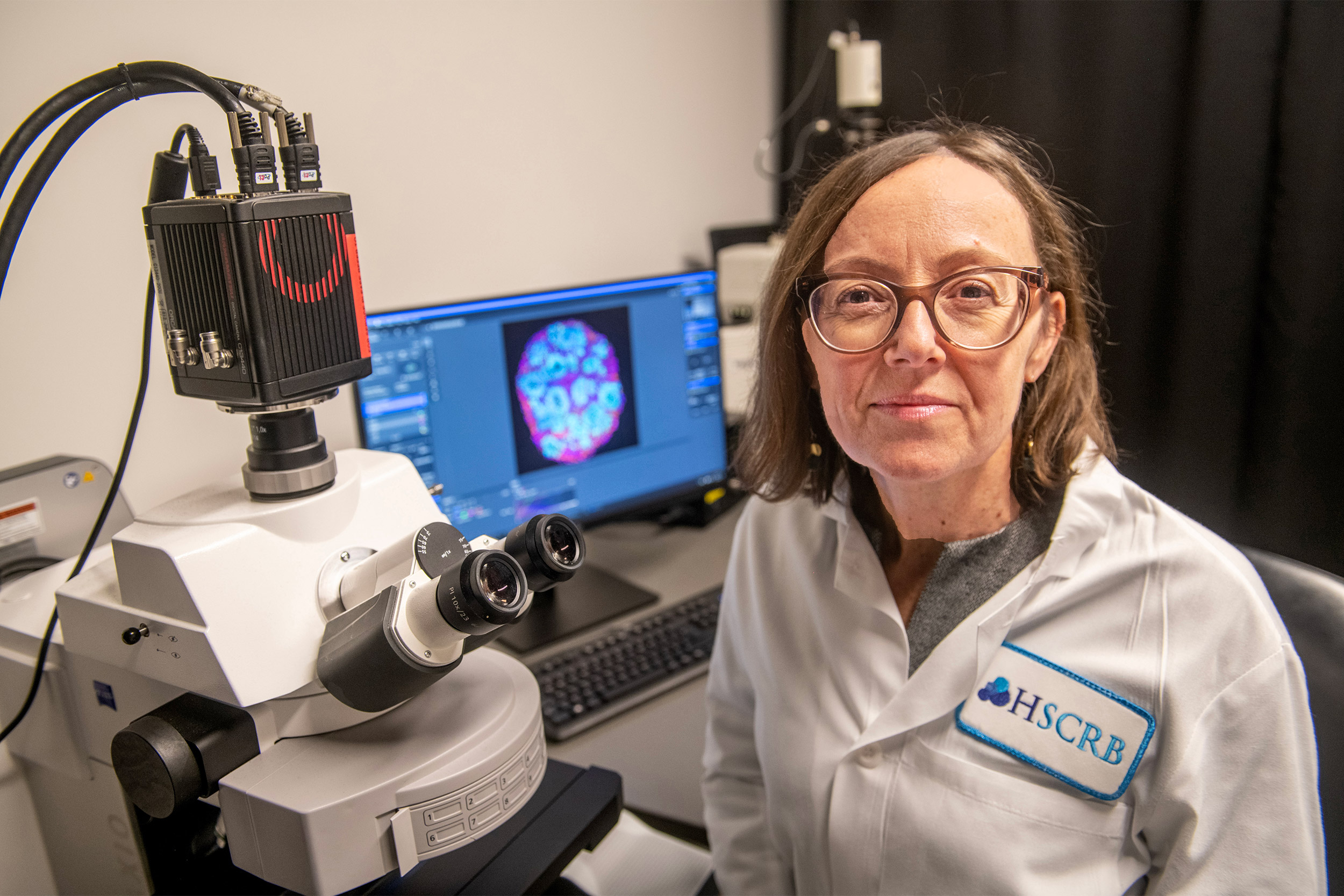
Paola Arlotta.
Harvard file photo
This research initiative is merely one illustration of the varied range of projects backed by the Bipolar Disorder Seed Grant Program of the Harvard Brain Science Initiative, a collaboration between the Faculty of Arts and Sciences (FAS) and Harvard Medical School (HMS). Over the past decade, the program has endorsed over 90 projects throughout the University and affiliated medical institutions and has hosted five symposia. In several instances, the grants have allowed researchers to devise innovative strategies that later secured larger funding from major funding bodies and led to publications in esteemed journals like Nature.
“The purpose of this grant program has always been to assist inventive scientists in our community in launching new research pathways concerning bipolar disorder,” stated Venkatesh Murthy, co-director of the Harvard Brain Science Initiative and Raymond Leo Erikson Life Sciences Professor of Molecular & Cellular Biology. “New paths, as well as new minds, are essential for comprehending and ultimately addressing this detrimental disorder.”
The program commenced in 2015 with the initial donation from the Dauten Family Foundation and has recently expanded due to a new contribution from Sandra Lee Chen ’85 and Sidney Chen. Kent Dauten, M.B.A. ’79, and his spouse, Liz, became involved after two of their four children were diagnosed with bipolar disorder, despite no known family history of the condition. “The field is severely underfunded and for far too long it has been a discouraging area of science due to the complexity of these brain disorders, but in recent years it has transformed into an exciting domain for discovery,” remarked Kent Dauten. The Chens were driven by similar motivations. “Bipolar disorder has impacted our family,” noted Sandra Chen. “Our experiences fuel our dedication to enhance understanding of what triggers this disruptive disorder.”
The program currently allocates $174,000 to each project over a two-year period. The 11 projects funded this year will explore bipolar disorder from various angles, including genetics, brain circuits, sleep, immune dysfunction, stress hormones, and gut microbiota.
The seed grants aim to foster “innovative ideas,” Murthy noted. He also stated, “Many of our grant recipients have made significant advancements with this support.”
An unresolved challenge
Bipolar disorder typically emerges during adolescence, and on average, individuals endure symptoms for nine years before receiving a diagnosis. It results in recurrent episodes of mania and depression — predominantly the latter.
The standard treatment includes mood stabilizer medications such as lithium. Some individuals are prescribed antipsychotic drugs, yet these may lead to weight gain.
The disorder frequently brings additional health issues such as cardiovascular diseases, Type 2 diabetes, metabolic syndrome, and obesity. Patients have a life expectancy that is 12 to 14 years lower than average, coupled with elevated rates of suicide.
The origins of bipolar disorder remain unclear, but it appears to stem from a intricate combination of genetic, epigenetic, neurochemical, and environmental elements.
Fundamental science: When brain signaling falters
Severe mood fluctuations are characteristic of bipolar disorder. Patients often alternate between manic phases (marked by grandiosity, risky behaviors, excessive talking, distractibility, and decreased need for sleep) to depressive phases (gloomy moods, lack of joy, weight variations, exhaustion, inability to focus, indecisiveness, and suicidal thoughts).
Nao Uchida, a professor of molecular and cellular biology, believes that one factor contributing to this instability is dopamine, a neurotransmitter that is crucial for learning, memory, movement, motivation, mood, and attention.
Uchida examines the role of dopamine in animal learning and decision-making. Dopamine is frequently referred to as the brain’s “reward system,” but Uchida proposes it is better understood as a mediator of predictions and their results. Mood is often reliant on not just the result itself, but rather on how much the outcome deviates from expectations — referred to by scientists as the reward prediction error (RPE).
A
“`
A few years back, Uchida became curious about how the dysregulation of the dopamine system might provide clues regarding the fluctuations of bipolar disorder.
“We had not conducted any research connected to these conditions previously, so this seed grant truly permitted me to enter the domain,” Uchida stated.
The funding enabled his laboratory to examine how the alteration of depressive or manic states influenced the responses of dopamine neurons in rodents. The team integrated recent discoveries about how synapses can be strengthened or weakened to enhance specific pathways. Some of their initial results will soon be featured in Nature Communications.
Uchida theorizes that the disorder could be associated with distorted signaling of the neurotransmitters involved in prediction and learning. When dopamine levels are elevated, an individual might become inclined to focus on positive outcomes while neglecting negative ones — making them susceptible to risky behaviors or entering manic episodes. Conversely, when dopamine levels are diminished, individuals tend to concentrate excessively on negative outcomes, disregarding the positive aspects — and this negativity leads them toward depression.
“A significant portion of our future expectations is influenced by our experiences,” Uchida commented. “I believe that this mechanism may be disrupted in various conditions, including depression, addiction, and bipolar disorders.”
Nao Uchida (left) and Louisa Sylvia.
Harvard file photo; courtesy photo
Clinical research: Tackling obesity
Louisa Sylvia gained a close perspective on bipolar disorder in her first position after completing college. Serving as a clinical research coordinator in a bipolar center, she observed patients grappling with anxiety, depression, and other symptoms. Repeatedly, she noticed patients gaining weight following the prescription of medications.
“I rapidly became disheartened by the options available for those with bipolar,” recalled Sylvia, who is now an associate professor in the Department of Psychiatry at Mass General Hospital and HMS. “The choices were primarily medications — medications known for their serious side effects.”
Sylvia has dedicated her career to seeking improved alternatives. (She is also the author of “The Wellness Workbook for Bipolar Disorder: Your Guide to Getting Healthy and Improving Your Mood.”) Even with the most effective current medications and psychotherapy, numerous patients continue to struggle with depression and other adverse effects. To enhance standard treatments, she has aimed to create interventions involving nutrition, physical activity, and well-being.
One promising approach is time-restricted eating (TRE). Limiting meals to a specific timeframe — for example, from 8 a.m. to 6 p.m. — can lead to weight reduction, enhanced mood and cognition, and improved sleep quality.
With the support of the seed grant, Sylvia intends to conduct a trial to assess the effects of TRE on bipolar patients. The study will explore how the management of eating patterns influences weight, mood, cognition, quality of life, and sleep cycles. She will collaborate with Leilah Grant, an instructor at HMS and researcher at Brigham and Women’s Hospital who specializes in sleep and circadian physiology.
“For individuals who are experiencing depression or have challenges with motivation or energy, TRE is considered one of the simpler lifestyle modifications to adhere to,” said Sylvia, who also serves as associate director of the Dauten Family Center for Bipolar Treatment Innovation at MGH. “We’re essentially saying, ‘Don’t concentrate as much on what you consume, but rather when you consume it.’”
The seed grants aim to foster promising strategies that may not receive funding through other means. Sylvia can confirm the importance of this opportunity; she faced rejections for two TRE grant applications seeking federal funding.
“I view it as an innovation grant to explore something somewhat novel that may not get funded through conventional channels,” she explained.
Translational research: Brain avatars
Despite decades of study, the success rate of medications for treating bipolar disorder remains frustratingly low. Lithium, the primary first-line treatment, delivers full benefits to only about 30 percent of patients — yet three-quarters of them also experience significant side effects.
Animal models do not always correlate to human treatment. Among humans, the responses can vary widely; some individuals gain from drug therapies while others do not.
To tackle these limitations, Arlotta is developing an innovative method to test drugs on brain cells from individuals with bipolar disorder — without jeopardizing the patients themselves.
Her team has spent over a decade creating human brain organoids. They initiate the process by taking a single blood sample from a person. Since blood cells contain copies of our DNA, they hold the genetic instructions that guide development from fetus to adulthood. With a sequence of biochemical signals, these blood cells are reprogrammed to become stem cells. The team then employs another set of signals to replicate the natural process of cell differentiation to cultivate human brain cells — but as cell cultures outside the body.
“You can produce thousands and thousands of brain organoids from any single person,” Arlotta remarked. “If the blood originates from a patient with a disorder, then each cell within that organoid carries the genome and genetic risk profile of that individual.”
These “avatars” — each approximately five millimeters in diameter — contain millions of brain cells and hundreds of distinct cell types. “That is the only experimental model of our brain that science possesses today,” she stated. “It may not be feasible to explore the brain of a patient with bipolar disorder, but scientists could utilize their avatars.”
In preliminary studies, the Arlotta team generated brain organoids from stem cells from two groups of bipolar patients: “lithium responders” who benefit from the treatment and “lithium non-responders” who do not. The researchers will assess whether these organoids mirror the variances observed in living patients — and then utilize them to formulate more effective therapeutic medications.
However, Arlotta recognizes that no singular strategy serves as a cure-all. Since bipolar disorder remains enigmatic, the seed grant program is invaluable as it encourages multiple promising research avenues across disciplines.
“The program reflects the modesty of recognizing how little we understand about bipolar disorder,” said Arlotta. “Thus, we need to pursue numerous paths forward.”