For numerous individuals suffering from schizophrenia, various psychiatric disorders, or conditions like hypertension and asthma, adhering to a daily medication schedule can be challenging. To tackle this issue, researchers at MIT have designed a pill that can be ingested just once a week, gradually dispensing medication from within the stomach.
In a phase 3 clinical trial led by MIT spinout Lyndra Therapeutics, scientists utilized the weekly pill to administer a commonly prescribed medication for alleviating symptoms of schizophrenia. They discovered that this treatment schedule maintained stable drug levels in patients’ bodies and managed their symptoms effectively, comparable to daily drug doses. The findings are disclosed today in Lancet Psychiatry.
“We’ve transformed a medication that needs daily intake to once weekly, orally, using a technology that can be customized for a range of medications,” explains Giovanni Traverso, an associate professor of mechanical engineering at MIT, a gastroenterologist at Brigham and Women’s Hospital, an associate member of the Broad Institute, and a co-author of the study. “The capability to maintain a sustained drug level over an extended time frame, presented in a user-friendly system, simplifies ensuring patients adhere to their treatment.”
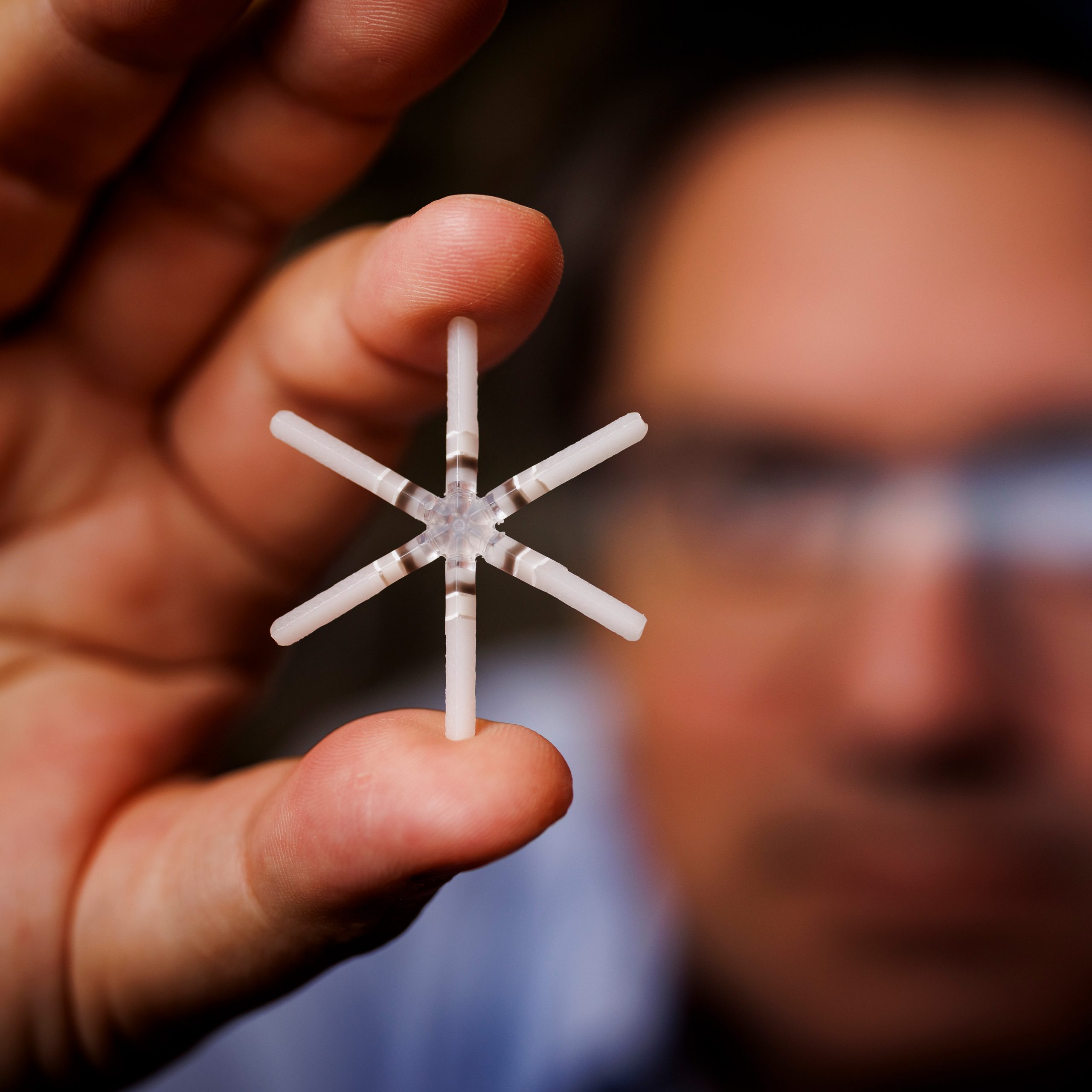
Traverso’s laboratory commenced the development of the ingestible capsule examined in this trial over a decade ago, as part of a continuous commitment to simplify medication administration for patients. The capsule is roughly the size of a multivitamin, and once ingested, it expands into a star-like shape that helps it stay in the stomach until the entire medication is provided.
Richard Scranton, chief medical officer of Lyndra Therapeutics, is the senior author of the paper, while Leslie Citrome, a clinical professor of psychiatry and behavioral sciences at New York Medical College School of Medicine, serves as the lead author. Nayana Nagaraj, medical director at Lyndra Therapeutics, and Todd Dumas, senior director of pharmacometrics at Certara, are also contributors.
Sustained delivery
Over the last ten years, Traverso’s lab has focused on developing a variety of swallowable capsules that can persist in the digestive system for days or weeks, gradually releasing their drug content. In 2016, his team introduced the star-shaped device, which was subsequently further refined by Lyndra for clinical trials involving schizophrenia patients.
This device features six arms that can fold inward, enabling it to fit inside a capsule. The capsule disintegrates when the device reaches the stomach, allowing the arms to deploy. Once the arms are extended, the device grows too large to move past the pylorus (the stomach’s exit), thus it remains suspended in the stomach while drugs are gradually released from the arms. After approximately a week, the arms detach independently, and each segment exits the stomach and continues through the digestive system.
For the clinical trials, the capsule was filled with risperidone, a widely utilized medication for treating schizophrenia. Most patients take this medication orally each day. There are also injectable variations available that can be administered bi-weekly, monthly, or every two months but necessitate healthcare provider intervention and may not always be preferred by patients.
The MIT and Lyndra teams opted to concentrate on schizophrenia, with the expectation that a less frequent drug administration, via oral delivery, could ease treatment for patients and their caregivers.
“One of the critical unmet needs recognized early was in neuropsychiatric conditions, where the illness can hinder or obstruct one’s ability to remember to take medications,” states Traverso. “Keeping that in mind, schizophrenia has been a significant focus of our research.”
The phase 3 trial was coordinated by Lyndra researchers and involved 83 patients across five different locations in the United States. Forty-five of these individuals completed the full five-week study, taking one capsule filled with risperidone each week.
Throughout the study, the researchers monitored the drug concentration in each patient’s bloodstream. Each week, they observed a prominent spike on the day the capsule was administered, followed by a gradual decrease in level over the subsequent week. All levels remained within the desired range, showing less fluctuation over time compared to when patients took a pill daily.
Effective treatment
Using a measure known as the Positive and Negative Syndrome Scale (PANSS), the researchers also determined that the patients’ symptoms stayed stable throughout the trial.
“A significant hurdle in the management of chronic illnesses is the inconsistent intake of medications. This can lead to worsening symptoms and, in schizophrenia cases, potential relapse and hospitalization,” comments Citrome. “The opportunity to take medication orally once a week provides a significant alternative that can enhance adherence for the numerous patients who prefer tablets to injections.”
Instances of side effects from the treatment were minimal, according to the researchers. Some patients experienced mild acid reflux and constipation early in the study, but these symptoms were short-lived. The outcomes, indicating the effectiveness of the capsule along with minimal side effects, mark a crucial advancement in this method of drug delivery, Traverso notes.
“This truly illustrates that what we speculated a decade ago—that a single capsule could serve as a drug reservoir within the gastrointestinal tract—is achievable,” he remarks. “What you observe here is that the capsule can reach the anticipated drug levels, while also managing symptoms in a significant group of patients with schizophrenia.”
The researchers are now aiming to conduct larger phase 3 studies prior to seeking FDA approval for this delivery method for risperidone. They are also preparing for phase 1 trials utilizing this capsule to administer other medications, including contraceptives.
“We are thrilled that this technology, which originated at MIT, has advanced to phase 3 clinical trials,” states Robert Langer, the David H. Koch Institute Professor at MIT, a co-author of the original star capsule study, and a co-founder of Lyndra Therapeutics.
The study received funding from Lyndra Therapeutics.