“`html
Health
Achieving significant progress in battle against Alzheimer’s
Scholars anticipate that innovative technologies and strategies may herald a period of viable treatments for this unmanageable illness in light of the pressing ‘silver tsunami’
Initially, it starts with misplaced keys. Then, there are overdue bills, conversations that fizzle out mid-way, and names that refuse to come to mind. Families, filled with a mix of apprehension and acceptance, pose the question to their physician: Could this be Alzheimer’s?
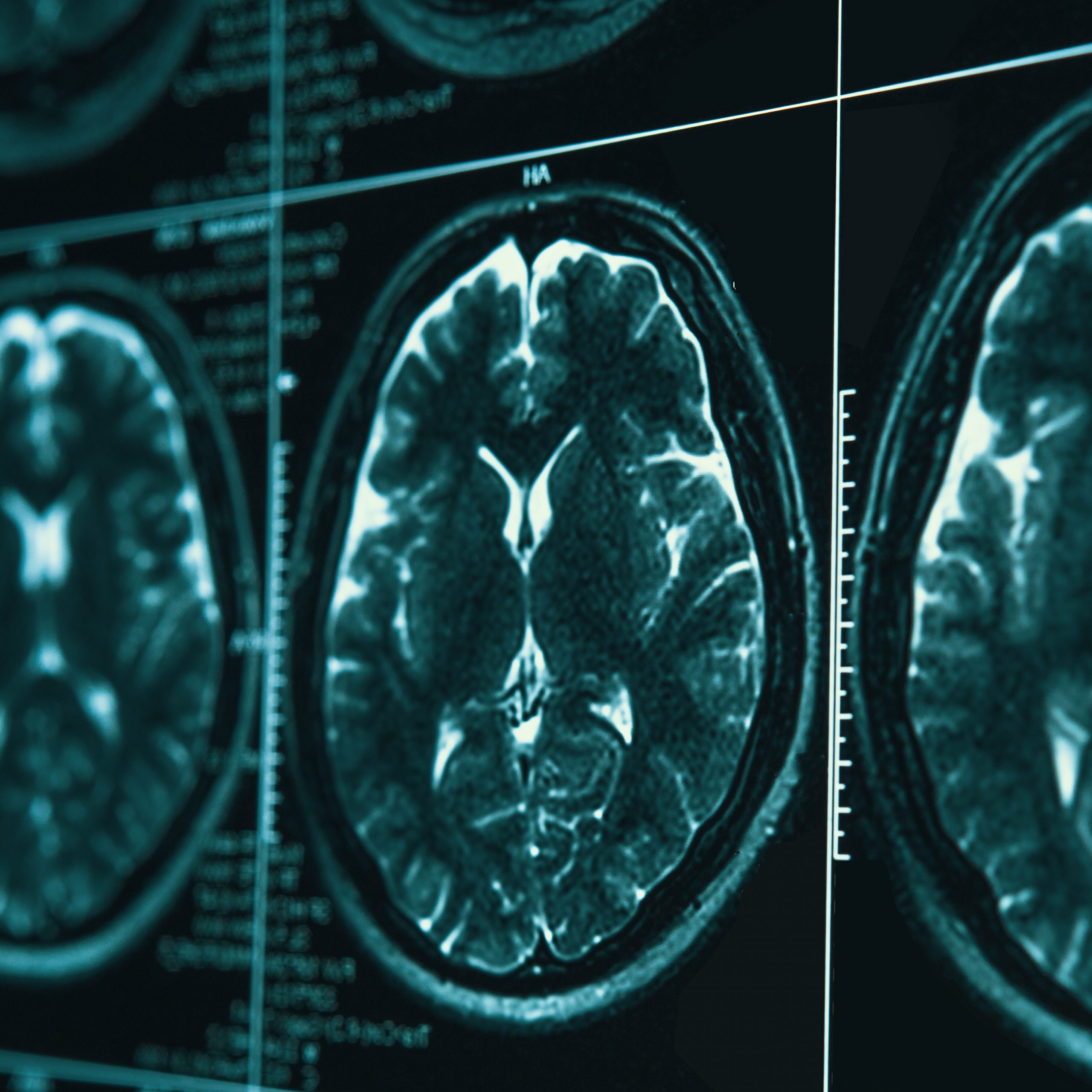
By the time the signs start causing issues, the ailment has been developing in the brain for years. Microscopic amyloid-beta plaques have built up between neurons, followed by strands of neurofibrillary tau proteins tangling into tight knots within brain cells. These two irregularities — first detailed in 1906 by German physician Alois Alzheimer — have come to symbolize the disease.
For years, scientists have pursued the question: If amyloid is a crucial element, could its removal halt or even reverse Alzheimer’s? The outcomes remain somewhat ambiguous. In clinical trials, FDA-sanctioned medications targeting amyloid plaques slow cognitive deterioration by approximately 30 percent but do not stop or reverse the ailment. Many possess the plaques yet show no symptoms.
However, cutting-edge technologies — artificial intelligence that may detect new genetic factors contributing to the ailment, blood tests for brain proteins, and real-time brain surveillance revealing how individual neurons perish — are uncovering novel methods to comprehend and potentially assist in treating Alzheimer’s.
Furthermore, recent investigations at Harvard Medical School and beyond are examining the possible influence of lithium deficiency as a factor leading to the onset and advancement of the illness.
This pursuit is urgent. As an increasing number of Americans enjoy longer lifespans, the population living with Alzheimer’s is projected to ascend from around 7.2 million in 2025 to roughly 18.8 million by 2050.
Though figures vary depending on methods, economic evaluations have estimated the total yearly healthcare expenses for Alzheimer’s and other forms of dementia to be about $1.5 trillion by 2050, compared to roughly $226 billion in 2015.
“We are currently facing the silver tsunami,” stated Steven Arnold, the lead researcher at the Alzheimer’s Clinical & Translational Research Unit at Massachusetts General Hospital. “If we cannot alter the trajectory of the disease medically, then our only genuine treatment becomes the physical and palliative care for seniors.”
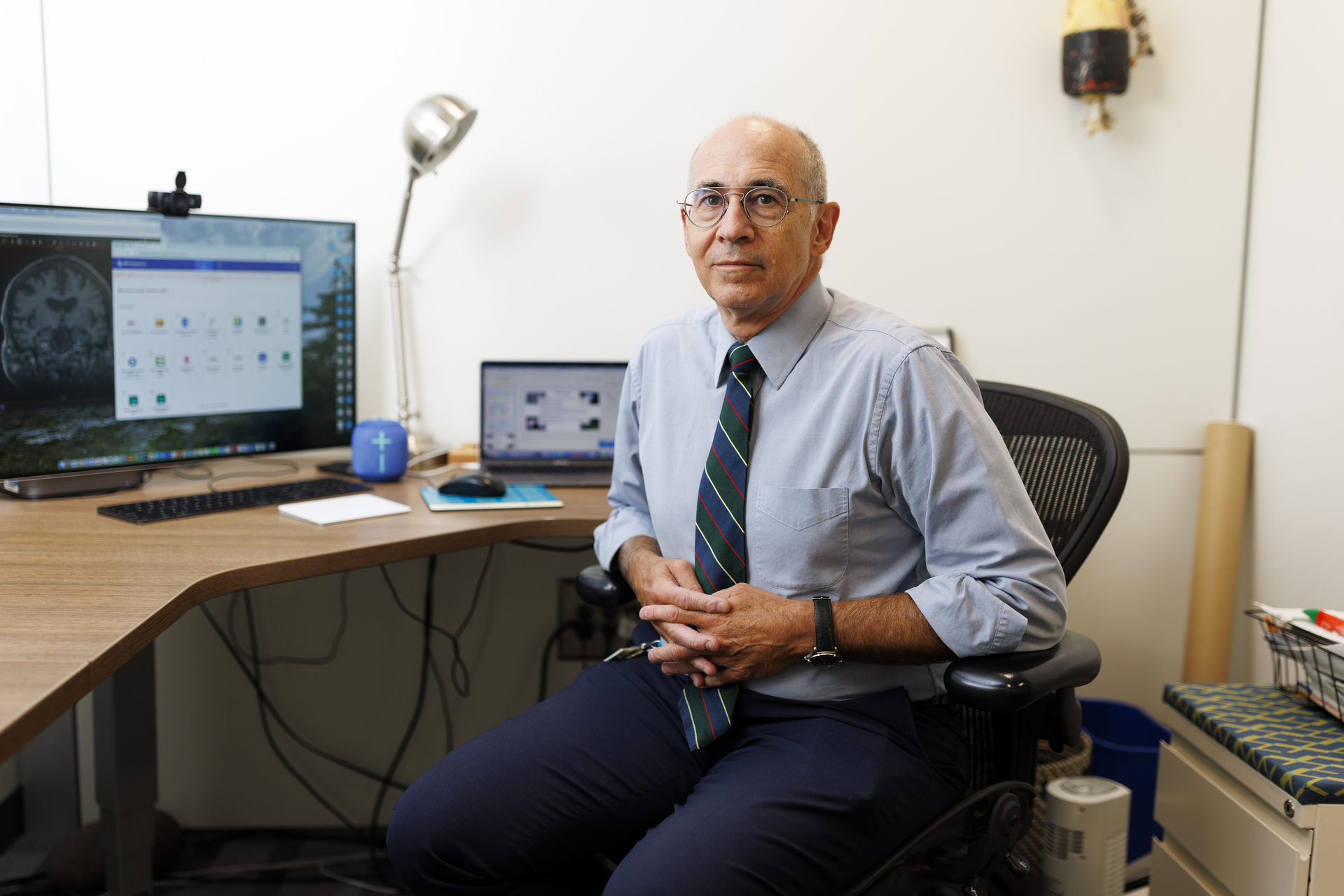
Steven Arnold.
Veasey Conway/Harvard Staff Photographer
Identifying the crucial moment
One of the perplexing aspects is that, while amyloid plaques constitute the primary condition of Alzheimer’s, individuals can coexist with these plaques for years, or even decades, without showing symptoms. Some never experience them.
Among individuals who fulfill the amyloid proteinopathy criteria for Alzheimer’s, merely 8 percent exhibit complete dementia, and only 17 percent show mild cognitive impairment, while 76 percent show no cognitive issues whatsoever.
Human brain tissue from the inferior temporal gyrus stained with fluorescent markers to highlight blood vessels (magenta) and amyloid beta protein plaques (white).
Video courtesy of MGH/HMS postdoctoral fellow Daniel Estrella, Ph.D.
Reisa Sperling, head of the Mass General Brigham Center for Alzheimer’s Research and Treatment, is focusing on the pivotal moment when an individual with benign amyloid suddenly manifests tau tangles, signaling cognitive decline. She refers to it as the “ca-tau-strophe.”
“It’s sort of an unusual play on words, but we refer to it as the cataustrophe because it is really associated with this swift spread of tau and impending cognitive decline. We’ve concentrated on: How do we foresee who’s going to experience this cataustrophe? Because that’s what we need to prevent.”
Her initial clinical trial, Anti-Amyloid Treatment in Asymptomatic Alzheimer’s Disease, or the A4 Study, was crafted to test this hypothesis. She enrolled over 1,100 individuals who had amyloid plaques but had not yet displayed clinical symptoms.
After 4.5 years, the anti-amyloid medication solanezumab did not substantially reduce plaque or slow disease progression. Even though the trial still added valuable insights into what is effective and what is not, it represented yet another setback.
Nonetheless, scientific inquiry requires thorough investigation. In an ongoing trial named AHEAD 3-45, Sperling is assessing a different antibody, lecanemab (the first FDA-sanctioned anti-amyloid treatment), even earlier in the course of the disease,
“““html
in cognitively normal individuals who demonstrate even lesser amyloid accumulation. The inquiry is: Can addressing amyloid sooner avert the disaster?
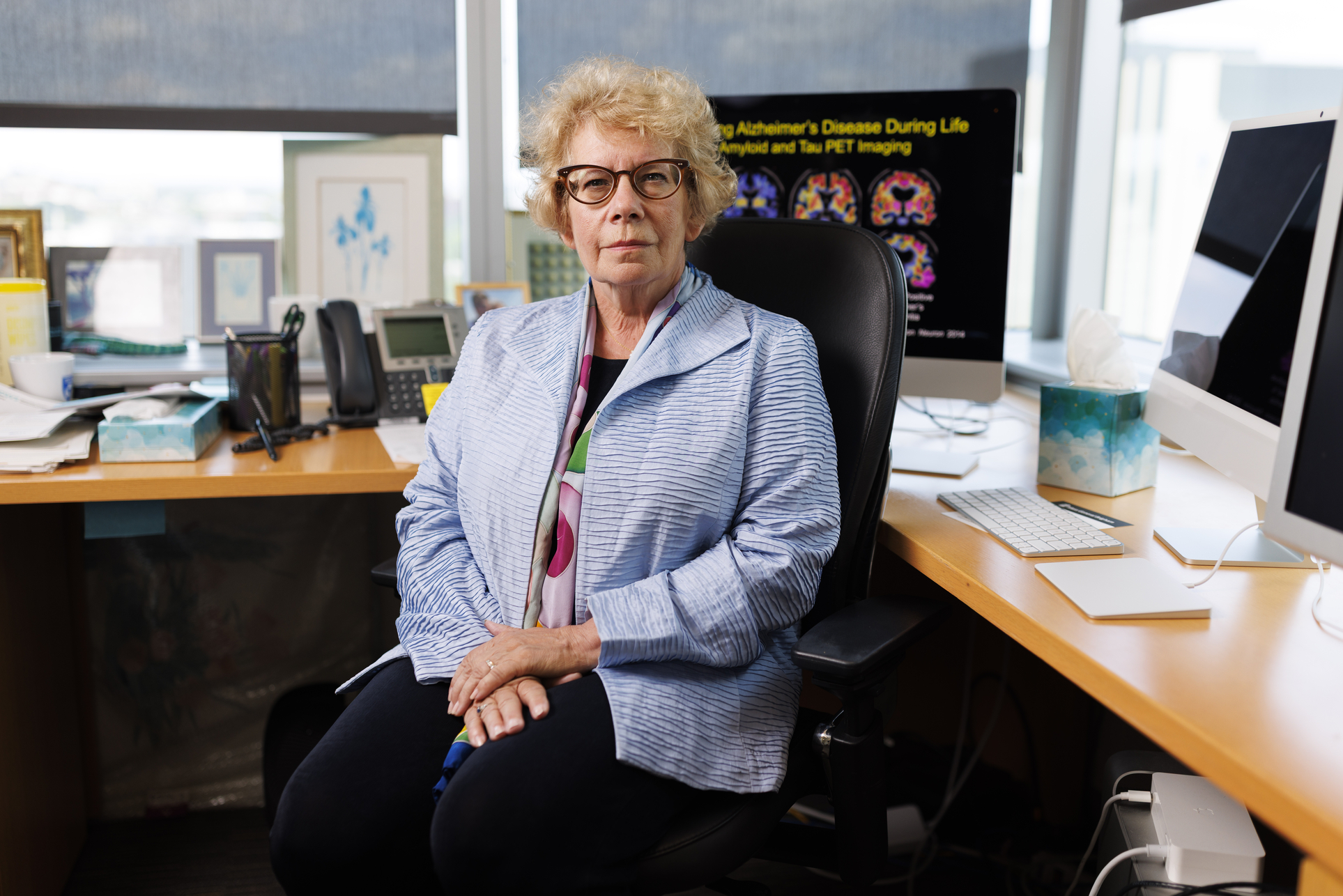
Reisa Sperling.
Veasey Conway/Harvard Staff Photographer
To ascertain if medications akin to those being evaluated by Sperling are effective, researchers require enhanced methodologies for monitoring the condition. This is where Ted Zwang’s contributions become significant. In a laboratory just nearby Sperling’s, Zwang employs adaptable brain electronics in murine models to attain a clearer understanding of the molecular foundation of the disease over time.
“We can observe both neurons and tau aggregates, noting what alterations occur from week to week, and we can pinpoint neurons that are perishing.”
If Zwang’s research successfully translates from mice to humans, it could enable the assessment of whether the anti-amyloid medications that Sperling is investigating are effective in real time.
“Instead of relying on amyloid PET or tau PET scans, what if we had a marker specifically for neurons that are in the process of dying?” Zwang remarked. “That would provide a considerably more straightforward approach to gauge if a treatment is beneficial.”
Ted Zwang.
Photo by Anna Olivella
The transition to a more accurate, data-driven methodology is also the emphasis for MGH data scientist Sudeshna Das. She employs artificial intelligence to sift through extensive datasets for fresh insights.
Her team’s multiscale graph neural network (GNN) model, named ALZ-PINNACLE, encompasses nearly 15,000 proteins and over 200,000 interactions spanning seven cell types, creating a more intricate portrayal of the illness.
Through her analysis of big data, Alzheimer’s appears less like a singular condition and more like an array of overlapping subtypes.
“Though characterized by amyloid and tau, numerous other genes and pathways exist: Genetics, metabolism, vascular health, inflammation, and even psychosocial elements like depression and isolation all contribute. We define it as a biopsychosocial illness,” she stated.
Das asserts that successful treatment hinges on differentiating Alzheimer’s subtypes. With AI, she believes these subtypes could be discerned in the upcoming years. This method would steer the field towards genuinely personalized medicine.
Investigating routes to resilience
While certain researchers pursue Alzheimer’s treatments, others concentrate on resilience— a combination of behaviors and characteristics that seem to guard against developing the disease.
Research indicates that individuals who inherit a rare version of the Apolipoprotein E gene, termed ApoE2, are resistant to Alzheimer’s disease. Conversely, a different variant, ApoE4, elevates the risk up to 10-fold.
Research indicates that individuals who inherit a rare variant of the Apolipoprotein E gene, known as ApoE2, exhibit resistance to Alzheimer’s disease. On the other hand, another variant, ApoE4, significantly heightens the risk, potentially as much as 10-fold.
Bradley Hyman, John B. Penney Jr. Professor of Neurology at HMS, recently demonstrated that a mouse model predisposed to ApoE4 could be effectively treated, reversing much of the harm, by introducing ApoE2 through gene therapy methods.
“These techniques are already in clinical application for other conditions, but we have yet to apply ApoE2 in patients,” remarked Hyman, who also leads the Alzheimer’s disease research unit at the MassGeneral Institute for Neurodegenerative Diseases (MIND). “Nonetheless, it represents an exciting strategy, and we are diligently working on how to reintegrate a factor that nature has shown to be protective in rare individuals back to the general population.”
Years ago, a fortuitous encounter guided Steven Arnold toward a notably different avenue of resilience: immunotherapy. He came across a colleague, MGH endocrinologist Denise Faustman, who was investigating a century-old tuberculosis vaccine for Type 1 diabetes treatment.
“She suggested, ‘You should explore that in the brain,’” Arnold recollected.
Emerging evidence indicated that individuals who received the Bacillus Calmette-Guérin (BCG) vaccine, also utilized to treat bladder cancer, exhibited reduced all-cause mortality.
“It appeared to enhance the immune system to provide protection against a diverse range of conditions—not just infections, but autoimmune disorders, multiple sclerosis,” he remarked. “Then some epidemiological data began to surface indicating that individuals who received BCG demonstrated a lower occurrence of developing Alzheimer’s or Parkinson’s disease.”
His team had become intrigued by a specific type of over-inflammation observed in Alzheimer’s patients. As he articulated, immune cells in the brain fulfill a crucial dual function: They clear damaged tissue while also refining healthy brain connections.
“You do not want the immune system to be underactive. You do not desire it to be overactive,” he noted. “You want it to be appropriately active.”
“You do not want [the immune system] underactive. You do not desire it to be overactive. You want it to be appropriately active.”
Steven Arnold
In 2023, Arnold and his team, including Das, discovered that BCG immunotherapy for bladder cancer was associated with a 20 percent decrease in the risk of subsequent Alzheimer’s disease and related dementia, with the protective link being stronger in those aged 70 or older.
While earlier studies had connected the BCG vaccine with a diminished risk of dementia, those investigations were constrained by sample size, study design, or analytical techniques.
This is a promising beginning, but merely that.
Arnold is also examining additional elements that could aid in disease prevention: lifestyle choices.
“We acknowledge that many of the same cardiovascular and metabolic risk factors associated with heart attacks and strokes—high blood pressure, elevated cholesterol, diabetes, obesity—serve as influencers that can affect both the likelihood of developing Alzheimer’s and the disease’s manifestations,” he explained.
In a 2024 study, Arnold co-authored research revealing that over a 20-week span, intensive dietary and lifestyle modifications could enhance amyloid biomarkers in the brains of patients with early-stage dementia due to Alzheimer’s disease, and might even improve cognitive function.
The results support The Lancet’s 14 crucial modifiable lifestyle factors that contribute to Alzheimer’s, including limited education, hearing impairment, high LDL cholesterol, social isolation, depression, traumatic brain injury, and physical inactivity. Although each factor is a minor contributor individually, collectively, these factors could potentially avert or postpone up to 45 percent of Alzheimer’s instances if eliminated, according to a report from The Lancet in 2024.
Exploring innovative strategies
Recent research at Harvard, much of which is competitively funded by the National Institutes of Health, continues to unveil new pathways and treatment opportunities.
A 2023 publication by an international team led by Harvard Medical School researchers at MGH and Massachusetts Eye and Ear identified a novel genetic variant that shields against Alzheimer’s.
Bruce Yankner, a professor of genetics and neurology at the Blavatnik Institute at HMS, proposed a new theory this August, attributing lithium deficiency as an underlying factor of the disease. The findings, which were a decade in development, demonstrate that lithium, utilized for mood disorders, naturally exists in the brain and protects it from neurodegeneration.
Researchers found that as amyloid-beta begins to emerge in the early phases of the condition, it binds to lithium, diminishing its functionality. Treating mice with lithium orotate, which does not bind to amyloid-beta, reversed the disease and its symptoms.
Each fresh insight necessitates years of ongoing investigation—and funding—before medications can gain public approval.
Scientists like Zwang remain cautiously hopeful. “We are in an exceptionally transformative timeframe regarding understanding Alzheimer’s disease, owing to many innovative methods of observing real-time occurrences in living individuals,” he remarked. “Progress is occurring so swiftly, especially with these treatments being trialed and these models being developed, that I would not be astonished if we uncover some genuinely effective treatments in the next few years.”
“`