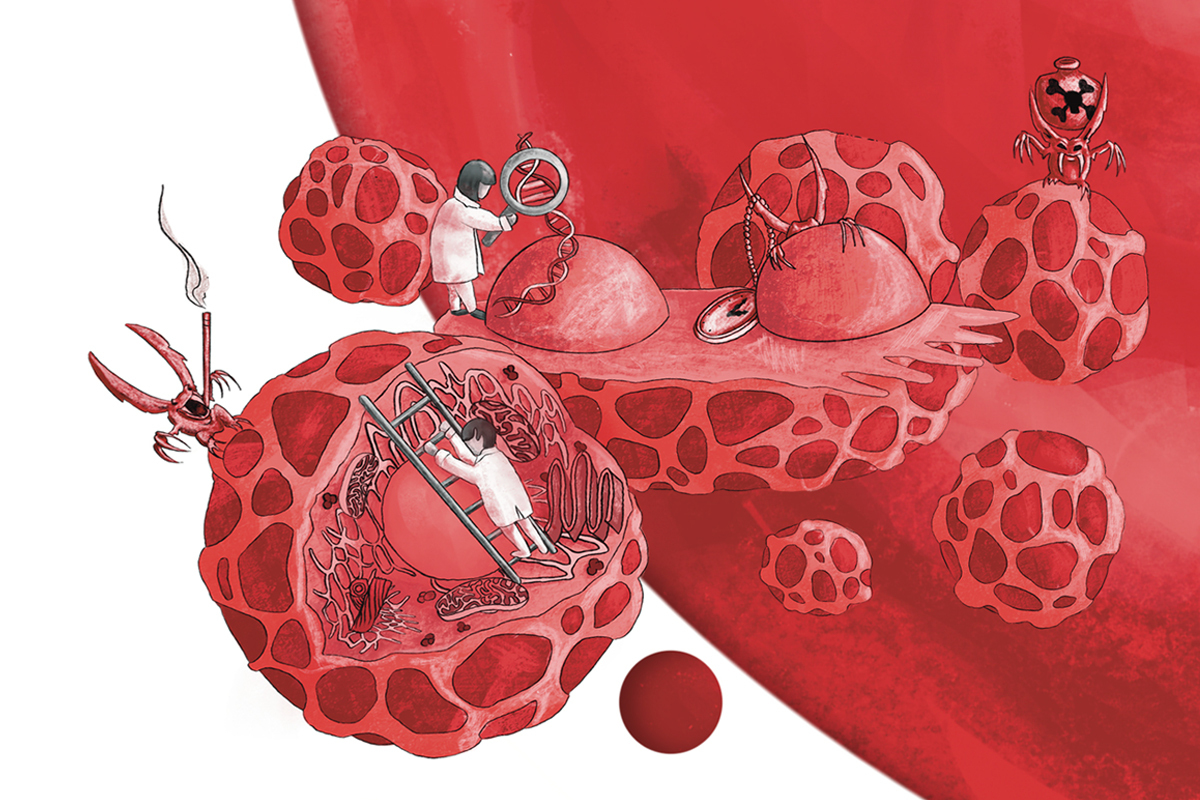
As we grow older, our cells divide, and the DNA within these cells can incur errors — or mutations — each time the sequence is replicated. The majority of newly formed mutations are benign, yet a few can shift the equilibrium towards cancer development as one ages.
Recently, a study spearheaded by researchers at Washington University School of Medicine in St. Louis has revealed that these newly formed mutations interact with our inherited mutations — those that come from our parents — in significant manners that affect a person’s lifelong cancer risk. Grasping these interactions could inform the creation of novel techniques for early detection and cancer prevention.
The investigation, featured in Nature Genetics, concentrated particularly on the risk related to blood cancers like acute myeloid leukemia (AML), although the interactions between inherited and acquired mutations likely play a part in other cancer types as well.
Inherited mutations are found in the egg and sperm and are thus present in every cell from birth, while acquired mutations accumulate steadily over time in various cells. Led by Kelly Bolton, MD, PhD, an assistant professor of medicine in the Division of Oncology at WashU Medicine and the senior author of the study, the research team aimed to understand how the interplay between these two mutation types affects a person’s risk of developing blood cancer.
Specifically, they investigated a blood condition known as clonal hematopoiesis, which is recognized for elevating the risk of blood cancer. Clonal hematopoiesis arises from a mutation in blood stem cells — cells that produce all the various cell types in the blood — granting those cells a slight survival advantage over normal stem cells. Such stem cell clones proliferate more and are at a heightened risk of evolving into blood cancer.
“The majority of individuals with clonal hematopoiesis never progress to blood cancer,” Bolton remarked, who treats patients at Siteman Cancer Center, affiliated with Barnes-Jewish Hospital and WashU Medicine. “To some degree, it’s a typical part of the aging process. However, we believe that many, if not all individuals who develop blood cancer pass through a phase of clonal hematopoiesis at some point. We are still in the initial phases of determining which individuals with clonal hematopoiesis will progress to blood cancer and which will not.”
Examining genomic data from over 730,000 individuals, including blood samples, the researchers discovered that clonal hematopoiesis was more prevalent among those with inherited mutations in specific genes already recognized to enhance cancer risk. They also found that these inherited mutations influenced the patterns of newly formed mutations responsible for clonal hematopoiesis. If stem cell clones acquire just a few more detrimental mutations, the clonal hematopoiesis can evolve into a blood cancer, such as AML, where the cells cease performing their functions and multiply until they displace healthy cells.
Aiming to discover methods to detect and eradicate pre-cancerous cells in high-risk individuals, Bolton and her team found that among those with clonal hematopoiesis, individuals with inherited mutations that predispose to clonal hematopoiesis faced a greater risk of developing blood cancer than those without inherited mutations.
“Our study represents an initial exploration of the inherited genetic background that forms the fertile ground, so to speak, and we’re observing which unwanted seeds acquired later in life are more or less likely to flourish from that background,” Bolton explained. “The objective is to eliminate the weeds early, before they can establish and become full-blown cancer.”
Although clonal hematopoiesis is a normal aspect of aging, various factors such as smoking or previous exposure to radiation or chemotherapy can accelerate the process and heighten the likelihood of it transforming into cancer. Nevertheless, some individuals progress to cancer even without significant environmental risk factors, and this new study indicates that the interplay between their inherited genome and newly acquired mutations significantly contributes to this cancer progression.
The lead author of the study, Jie Liu, a graduate student in Bolton’s lab, remarked: “It’s thrilling to see how combining large-scale genomic information can uncover how inherited and acquired mutations collaborate to affect cancer risk. These revelations move us closer to identifying high-risk individuals before cancer arises. Our findings illustrate that it’s not solely the mutations you’re born with or those you acquire later in life, but the interaction between them, which we can now quantify.”
Earlier Intervention
Bolton indicated that the ability to detect and quantify both inherited cancer risks and clonal hematopoiesis may be a potent approach to identify individuals who would gain the most from early preventive strategies, such as targeted therapies for the most harmful mutations. Currently, recognizing clonal hematopoiesis is challenging without specialized blood tests not routinely included in standard care. Even with existing clones comprising a larger portion of their blood stem cells, individuals can still exhibit normal blood cell counts in standard blood tests typically conducted during an annual health check-up, for instance.
In theory, if researchers identify the gene mutations to monitor, they could create new blood tests to recognize such individuals before any signs of a problem emerge through routine blood screening tests. The new study highlights numerous genes of interest that could be pivotal in the future development of such a blood test.
“Since leukemia is incredibly challenging to treat, we aspire to discover ways to intervene early — while it is still pre-cancerous — so we can prevent clonal hematopoiesis from evolving into leukemia,” Bolton stated. “We aim to initiate preventive clinical trials for individuals with certain inherited mutations who already exhibit evidence of clonal hematopoiesis, such as one or two clones expanding in their blood.”
Researchers at Siteman are currently conducting clinical trials examining whether specific drugs labeled IDH1 and IDH2 inhibitors can halt the expansion of certain blood stem cell clones before they develop into cancer. At this stage, such trials only include individuals deemed to have clonal hematopoiesis due to having already progressed to abnormal blood cell counts, positioning them on the verge of full-blown leukemia.
“We hold hopeful expectations regarding these preventive treatments, but we wish to possess tools to identify these individuals even earlier, before their blood cell counts sway from normal,” Bolton expressed. “Numerous targeted therapies are presently under development, and new avenues researchers are exploring for this purpose.”
Liu J, Tran D, Xue L, Wiley BJ, Vlasschaert C, Watson CJ, MacGregor HAJ, Zong X, Chan ICC, Das I, Uddin MM, Niroula A, Griffin G, Ebert BL, Mack T, Pershad Y, Sharber B, Berger M, Sehir A, Ptashkin R, Levine RL, Papaemmanuil E, Joseph V, Gao T, Kemel Y, Mandelker D, Stopsack KH, Pharoah PDP, Mukherjee S, Ding L, Cao Y, Walter MJ, Blundell JR, Chatterjee N, Offit K, Godley LA, Link DC, Stadler ZK, Bick AG, Natarajan P, Bolton KL. Germline genetic variation impacts clonal hematopoiesis landscape and progression to malignancy. Nature Genetics. July 15, 2025. DOI: 10.1038/s41588-025-02250-x.
This research was funded by the National Institutes of Health (NIH), grant numbers R01HL148050, R01HL168894, DP5 OD029586,
“`html
R01AG088657 and R01AG083736; the MDS Foundation; the Children’s Discovery Institute; a Prostate Cancer Foundation Challenge Award; the Edward P. Evans Foundation; the SciLifeLab & Wallenberg Data Driven Life Science Program, grant number KAW 2020.0239; the Swedish Cancer Foundation, grant numbers 22.0577JIA and 22.2362Pj; the Swedish Research Council, grant number 2023-03131; a Burroughs Wellcome Fund Career Award for Medical Scientists; a Pew Charitable Trusts and Alexander and Margaret Steward Trush Pew-Stewart Scholar for Cancer Research Award; and a Hevolution/AFAR New Investigator Award in Aging Biology and Geroscience Research. The examination was performed utilizing the U.K. Biobank Resource and data obtained from participants and gathered by the National Health Service. It also incorporated information from the All of Us Research Program of the National Institutes of Health. The material is solely the obligation of the writers and does not necessarily express the official perspectives of the NIH.
About Washington University School of Medicine
WashU Medicine is a worldwide pioneer in scholarly medicine, encompassing biomedical research, patient care, and educational initiatives with 2,900 faculty members. Its National Institutes of Health (NIH) research funding portfolio ranks second among U.S. medical schools and has expanded by 83% since 2016. Together with institutional funding, WashU Medicine dedicates well over $1 billion each year to basic and clinical research innovation and training. Its faculty practice consistently places within the top five in the nation, featuring over 1,900 faculty physicians operating at 130 sites. WashU Medicine’s doctors exclusively staff Barnes-Jewish and St. Louis Children’s hospitals — the academic hospitals of BJC HealthCare — and serve patients at BJC’s community hospitals across the region. WashU Medicine has a distinguished history in MD/PhD training, having recently allocated $100 million to scholarships and curriculum enhancement for its medical students, and hosts exceptional training programs across all medical subspecialties, as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website
The article Genetic study suggests ways to catch blood cancer earlier first appeared on The Source.
“`