Worldwide, and particularly in low- and middle-income nations (LMICs), a considerable segment of the populace is deprived of fundamental health-care services. Although there are numerous factors that contribute to hindrances in access, in many LMICs, malfunctioning or outdated equipment significantly contributes to the problem.
“Those of us who have explored health-care systems in LMICs are acquainted with what are referred to as ‘equipment graveyards,’” states Nevan Hanumara SM ’06, PhD ’12, a research scientist in MIT’s Department of Mechanical Engineering, depicting heaps of inoperative, imported apparatus, frequently marked with labels from donor organizations.
“Investigating the underlying reasons for medical equipment breakdowns and their abandonment in LMICs, we discover that local biomedical engineers genuinely cannot perform the maintenance due to a series of obstacles,” he explains.
Among these obstacles are: design flaws—devices designed for temperate, air-conditioned settings and stable power often struggle in environments with unreliable power sources, dirt, high temperatures, and humidity along with constant use; issues with supply chains—components ordered in the U.S. can arrive in days, whereas parts requested for East Africa may take months; and restricted access to skilled professionals—beyond major urban centers, biomedical engineers are quite rare.
Hanumara, along with Leroy Sibanda SM ’24, a recent dual-degree graduate in management and electrical engineering and computer science (EECS), and Anthony Pennes ’16, a technical instructor in EECS, began to consider what could be altered if local biomedical engineers were actively engaged in the design of the equipment they are responsible for maintaining.
Pennes, who teaches course 2.75/6.4861 (Medical Device Design), among other subjects, created practical biosensing and mechatronics activities for class exercises a few years ago. Hanumara sought to expand that curriculum to create something capable of having a larger influence.
Collaboratively, and with backing from MIT International Science and Technology Initiatives (MISTI), the MIT Jameel World Education Lab, and the Priscilla King Gray Public Service Center, the trio developed a hands-on course, activities, and curriculum, supported by what they now refer to as a “Biomed Lab in a Box” kit.
Sibanda, originally from Bulawayo, Zimbabwe, adds valuable personal experiences to the project. He mentions friends across the continent speak about excellent practical primary and secondary education, and a tertiary education heavily reliant on theory. The result, he notes, is a multitude of graduates who excel in theoretical knowledge but lack practical experience in advanced concepts.
“Anyone who has ever needed to create systems that endure real-world conditions understands the gap between understanding how to compute the theoretically ideal ‘x’ and being able to implement a viable solution with the available materials,” asserts Sibanda.
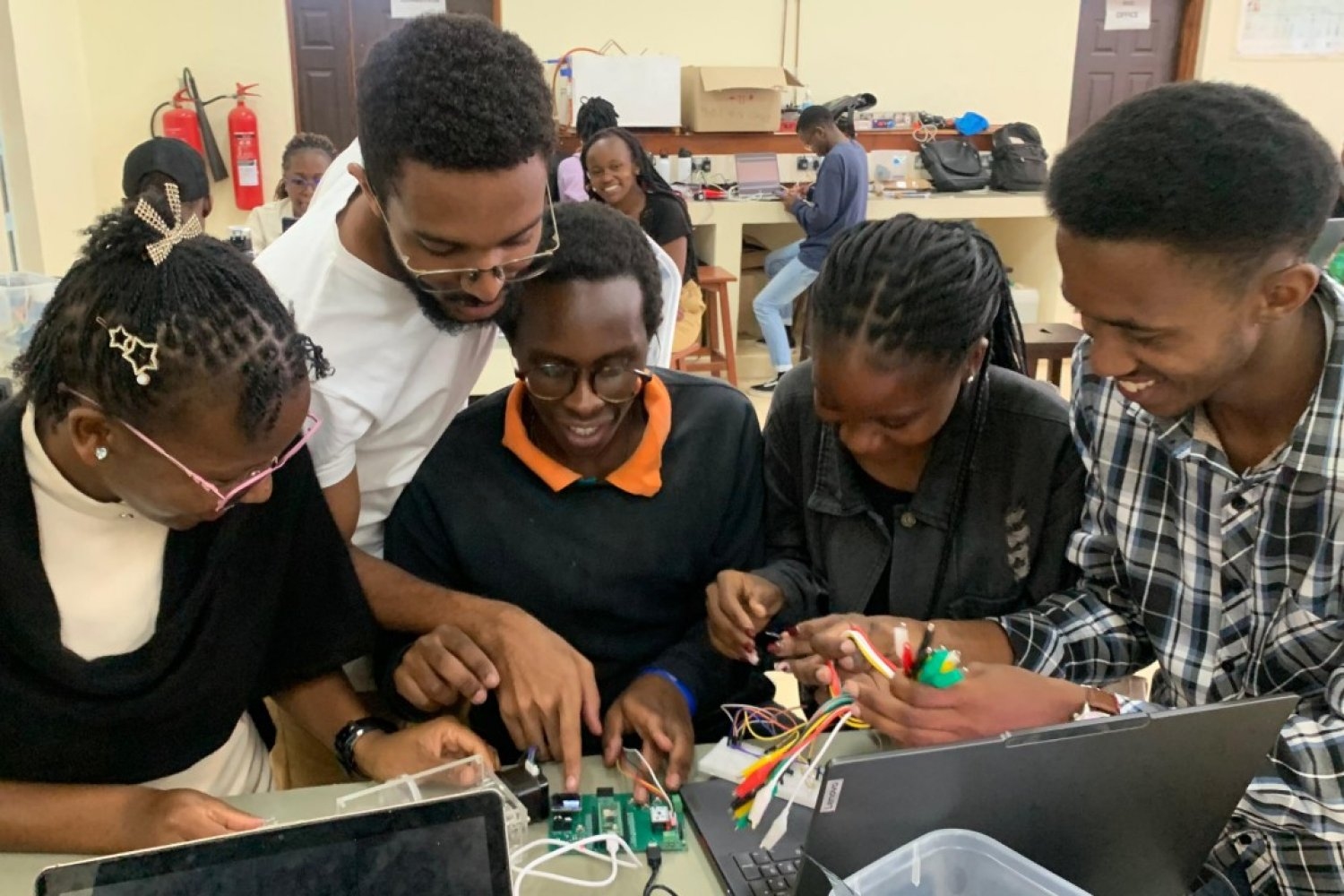
Hanumara and Sibanda journeyed to Nairobi, Kenya, and Mbarara, Uganda, in late 2024 to test their kit and validate their hypothesis, offering three-day biomedical innovation mini-courses at both Kenyatta University and Mbarara University of Science and Technology (MUST), with Pennes providing remote assistance from MIT’s campus.
The curriculum, based on 2.75, featured labs designed to link the theoretical aspects to physical applications, increasing in complexity and exposing students to the genuine challenges posed by biomedical hardware and sensing, such as weak signals, ambient noise, motion artifacts, debugging, and meticulous assembly.
Pennes states that the aim of the mini-courses was to align the project with the real-world experiences of the region’s biomedical engineering students. “One of the difficulties they face in this area is not merely a shortage of equipment but also the inability to maintain it,” he explains. “Occasionally, an organization will contribute thousands of dollars worth of surgical lighting; then a power supply fails, and the organization never returns to rectify the issue.”
However, he highlights that this is merely the start of the problem. Engineers often realize that the design is not transparent, and there is no manual, rendering it impossible to access a circuit design for the components inside the donated, proprietary system. “You have to explore the disassembled equipment to discern the makers’ original objectives in wiring it, and find a solution,” Pennes elaborates.
In one particular instance, he recounts observing a donated screen for viewing X-rays—the lightbox type used to illuminate film for technicians to analyze the image—with a burnt-out bulb. “The screen depends on a proprietary bulb, so when it burned out, they could not substitute it,” he recalls.
Local biomedical engineers eventually discovered they could utilize a number of standard fluorescent bulbs and adjust their angles to fit inside the box. “Then they sort of MacGyver’d the wiring to make them all functional. You get the medical technology to operate however you can,” he remarks.
It’s this practical, inventive approach to problem-solving that the team aspires to foster—and it’s a method that is very much in line with MIT’s ethos. “We’re not just people with ideas, where we write a paper and conclude it; we want to see it implemented,” says Hanumara. “This is why numerous startups emerge from MIT.”
Course modules offered at Kenyatta and MUST included “Breadboarding an optical LED – photodetector pulse detector,” “Soldering a PCB and testing a 3-lead EKG,” and “Assembling and programming a syringe pump.” Each module is structured to be a standalone learning experience, and the kit comes with a USB flash drive containing a 96-page lab manual authored by Sibanda, along with all necessary software, which is crucial when internet connectivity is unstable. The third activity related to the syringe pump is accessible via open access from the journal Biomedical Engineering Education.
“Our objective was to introduce enthusiastic, young biomedical engineers to the hands-on, ‘mens-et-manus’ (‘mind-and-hand’) culture that forms the foundation of MIT, and encourage them to nurture their skills and aspirations as engineers and innovators,” states Hanumara. “We aimed to empower them to take part in developing high-quality, contextually relevant technologies that enhance healthcare delivery in their own region.”
A LinkedIn post authored by Hanumara shared reflections from students regarding their experiences with the material. “Every lab—from pulse oximetry and EKGs to syringe pump prototyping—brought classroom concepts to life, illustrating the real-world applications of what we learn,” wrote Muthoni Muriithi, a student at Kenyatta University. “Utilizing breadboards, programming microcontrollers, soldering components, and analyzing biological data in real time helped me comprehend the extent of careful planning and precision involved in creating reliable healthcare instruments.”
Student feedback from both institutions is already aiding in refining the materials and planning future pilot programs.
Sibanda emphasizes another crucial aspect the team is monitoring—what transpires beyond the sessions after instructors depart. “It’s not merely about providing the resources,” he states. “It’s vital to comprehend what students deem most valuable, especially on their own.”
Hanumara agrees. “[Pennes] designed the core board we are utilizing to be multifunctional. We didn’t modify any of the features he integrated—we are eager to observe what students will accomplish with them. We also want to see how they can leverage the mental framework,” he says, noting that this strategy is essential for empowering students to explore, innovate, and ultimately elevate their own concepts.
Moreover, the project addresses another challenge identified early on: supply chain difficulties. In alignment with the mission of enhancing local capabilities, the entire kit was assembled in Nairobi by Gearbox Europlacer, which operates the only automated circuit board line in East Africa and is authorized to manufacture Raspberry Pi’s microcontrollers. “We did not inform the students of anything,” says Hanumara, “but allowed them to recognize that their circuit boards and microcontrollers read ‘Made in Kenya.’”
“The emphasis on local manufacturing prevents us from falling into the trap that much donated equipment creates in East Africa—you obtain one of these devices, and if any component fails, you can never replace it,” states Pennes. “Utilizing locally sourced materials means that if another component is required, or if you craft an intriguing side project, you have a shopping list to acquire whatever you need.”
“Building upon our ‘Biomed Lab in a Box’ initiative,” states Hanumara, “we aspire to collaborate with our colleagues in East Africa to further explore what can be designed and produced with the eager, young talent and abilities in the region.”
Hanumara’s LinkedIn update also expressed gratitude to collaborating professors June Madete and Dean Johnes Obungoloch, from Kenyatta and MUST, respectively, as well as Latiff Cherono, managing director of Gearbox. The team hopes to ultimately release the entire course in an open-source format.