“`html
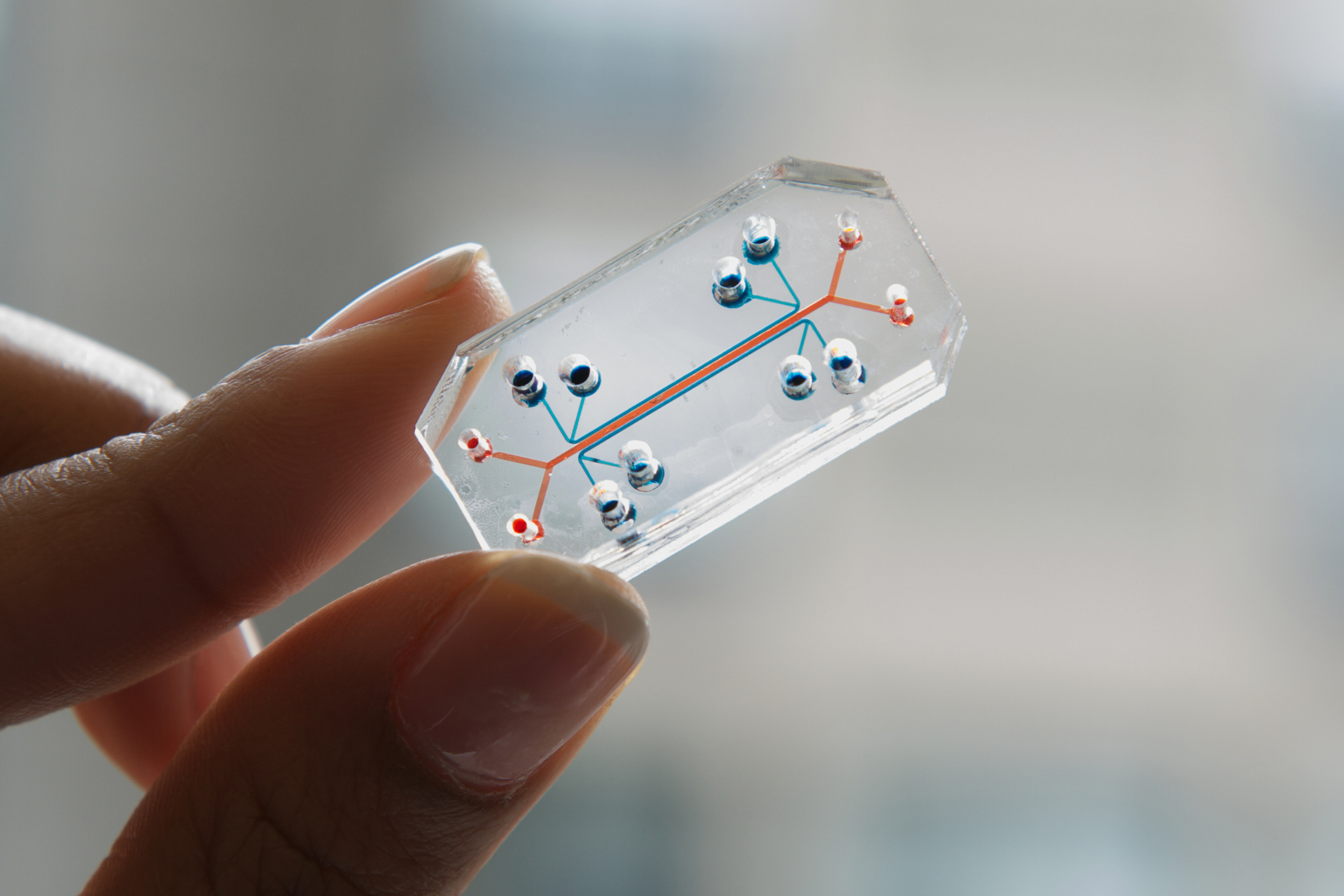
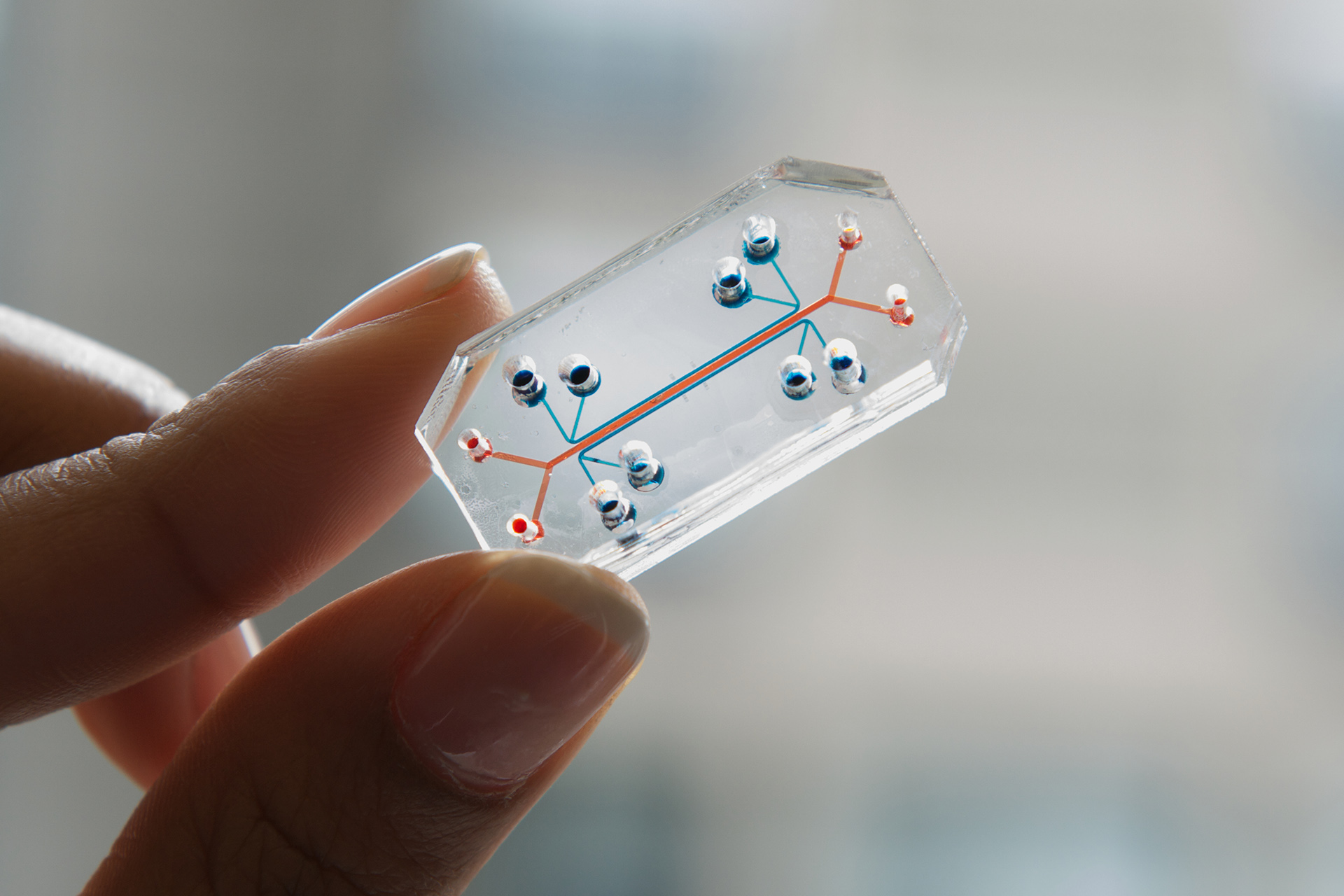
The Wyss Institute has crafted “organ chips” for the lungs, intestines, vagina, cervix, and fallopian tubes, among various others.
Wyss Institute
Health
A condition more prevalent than asthma or diabetes, yet frequently overlooked
Females experiencing severe menstrual bleeding typically wait five years on average before receiving care. Wyss technology could transform this situation.
Every minute, a woman in the U.S. requires a blood transfusion due to heavy menstrual bleeding, or HMB. One in three women reports having the condition — which can result in iron deficiency and anemia — and missing an average of 3.6 weeks of work a year, costing the U.S. economy approximately $94 billion yearly, as stated by the nonprofit Wellcome Leap. Patients typically endure for up to five years before receiving assistance, despite HMB being more prevalent than asthma or diabetes in women of reproductive age.
Despite the condition’s prevalence and severity, its origins remain inadequately understood.
To fill this void, Donald Ingber, founding director of the Wyss Institute and the Judah Folkman Professor of Vascular Biology at Harvard Medical School and the Vascular Biology Program at Boston Children’s Hospital, is working on the first human model of HMB. In September, the institute announced that it had obtained funding from Wellcome Leap’s $50 million Missed Vital Sign program to develop an organ-on-a-chip model of menstruation, utilizing the platform Ingber initially created at the Wyss in 2010.
The aim? Decrease the duration it takes for a woman to secure effective treatment for HMB from an average of five years to five months — more than tenfold.
“Women’s health has been neglected for such a long time — and that extends far beyond reproductive health,” Ingber stated. “This technology can dismantle that inequality and emphasize women’s health in a direct manner.”
An organ on a chip is essentially a “living, 3D cross-section of a primary functional unit of an organ,” clarified Ingber, who is also the Hansjörg Wyss Professor of Biologically Inspired Engineering at the School of Engineering and Applied Sciences.
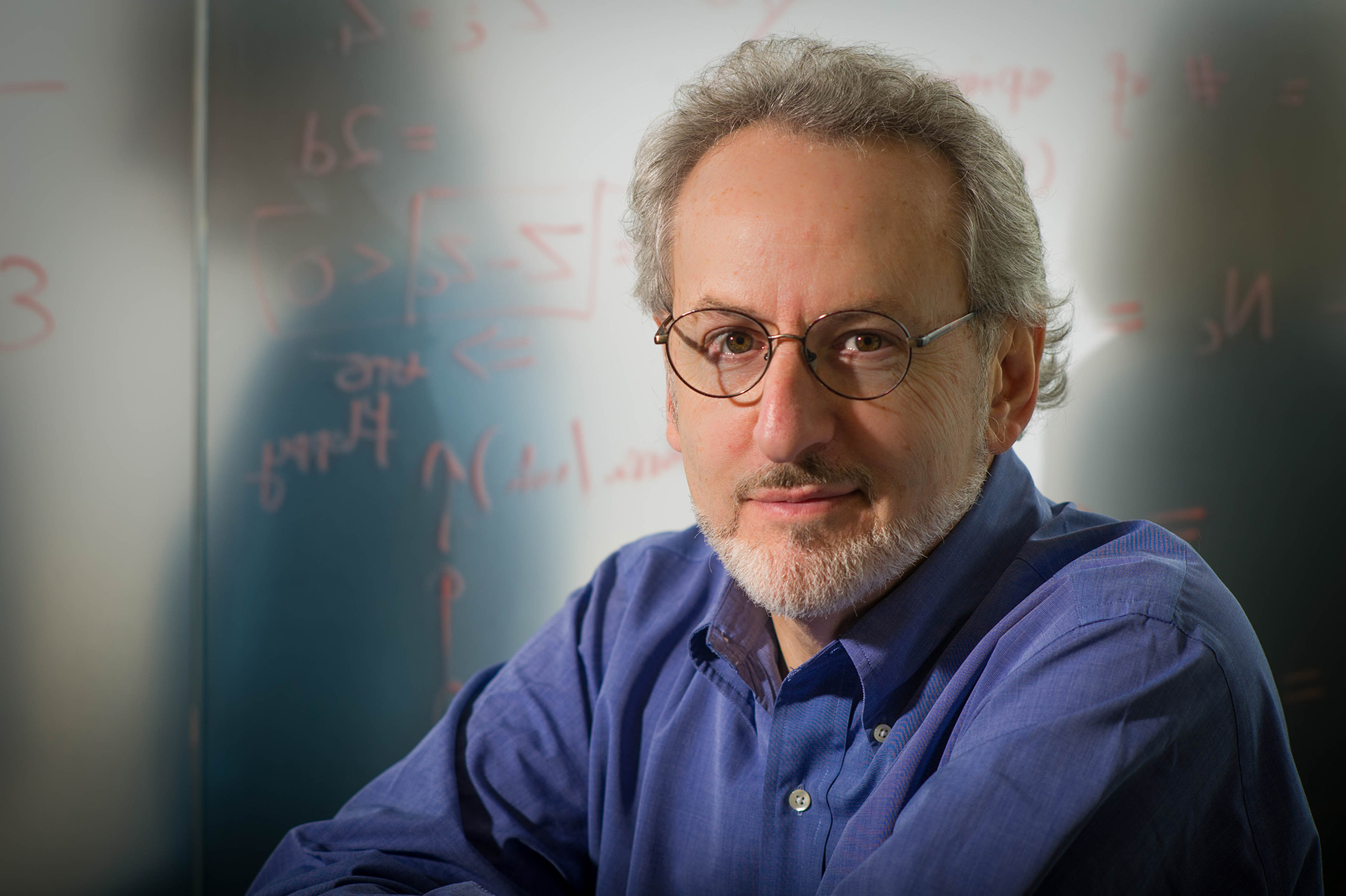
Donald Ingber.
Wyss Institute
The chips enable researchers to isolate the intricate, interconnected functions of the human body to study one component at a time. His lab has already created effective organ chips for the lungs, intestines, vagina, cervix, and fallopian tubes, among other organs.
Ingber intends to utilize the new menstruation organ-on-a-chip model to investigate a variety of potential factors, including genetic variations, hypoxia or low-oxygen circumstances, microbiomic influences, and inflammation. However, first, he and his team must construct the model.
“I always advise my graduate students, you should aim to condense a problem down to a single molecule,” Ingber elaborated. “What constitutes an organ is two or more tissues that merge, resulting in new functions. … So can we simplify something as intricate as organ physiology?”
The chips function by isolating a small segment of organ-level operation within a controlled setting. Each chip features two parallel channels divided by a porous membrane. One channel contains live human vasculature lined with endothelial cells — the same type of cells that constitute the inner walls of capillaries and regulate the exchange of nutrients, gases, and waste — and in some instances connective tissue cells that offer support for overlying lining cells in the body. The adjacent channel is lined with organ-specific epithelial cells that correspond to various organs, including those forming the reproductive tract. Researchers can introduce different stimuli into either channel and monitor how the tissues respond. Side channels can be employed to apply suction, stretch, and compress the tissue to mimic movements such as breathing and peristalsis.
“We possess the capability to control a multitude of parameters individually,” Ingber noted. “Is it precisely like in vivo? No. But that’s the essence of every model: It’s an approximation, and it’s significantly better than an animal model.”
The comparison to an animal model is relevant. Except for a species known as the Cairo spiny mouse, mice do not menstruate. Instead, they undergo what is termed an estrous cycle, during which the endometrium — the lining of the uterus — gets reabsorbed into the body.
This biological distinction presents a genuine challenge for medical research. Mice are extensively used in preclinical studies because their biology shares notable similarities with that of humans. However, when it comes to analyzing the human menstrual cycle, including disorders such as heavy menstrual bleeding, conventional animal models are inadequate — contributing to disparities in research concerning women’s health.
As part of its comprehensive initiatives to mitigate disparities in women’s health, the Wyss Institute hosts the Women’s Health Catalyst, a research center that has spearheaded work in areas such as lactation, early detection of ovarian cancer, and enhancement of endometriosis treatment, among other projects. Ingber remarked that the organ-on-a-chip has the potential to transform research into overlooked areas of women’s reproductive health.
“`