A widely used sleep medication reinstates healthier sleep cycles and shields mice from the neurological damage observed in degenerative brain conditions, such as Alzheimer’s disease, according to fresh findings from Washington University School of Medicine in St. Louis. The medication, lemborexant, inhibits the detrimental accumulation of an irregular variant of a protein known as tau in the brain, mitigating the inflammatory brain damage tau is notorious for causing in Alzheimer’s.
The research indicates that lemborexant and other medications that function similarly might assist in managing or preventing the harm inflicted by tau across various neurodegenerative disorders, including Alzheimer’s, progressive supranuclear palsy, corticobasal syndrome, and certain frontotemporal dementias.
This study was published on May 27 in Nature Neuroscience.
“We have been aware for quite some time that insufficient sleep is a risk factor for Alzheimer’s disease,” stated senior author David M. Holtzman, MD, the Barbara Burton and Reuben M. Morriss III Distinguished Professor of Neurology at WashU Medicine. “In this new research, we have demonstrated that lemborexant enhances sleep and diminishes abnormal tau, which seems to be a primary contributor to the neurological harm observed in Alzheimer’s and several related conditions. We are optimistic that this discovery will lead to additional investigations of this sleep medication and the creation of new therapies that may prove to be more effective than current alternatives, whether used alone or in combination with other existing treatments.”
“The antibodies targeting amyloid, which we currently employ to manage patients with early, mild Alzheimer’s dementia, are beneficial, but they do not slow the disease’s progression as much as we would prefer,” he continued. “We require methods to decrease the unusual tau accumulation and its related inflammation, and this type of sleep aid warrants further examination. We are intrigued to see whether addressing both amyloid and tau through a combination of treatments could yield more effective results in hampering or halting the progression of this disease.”
Holtzman and his group were among the pioneers in recognizing the relationship between inadequate sleep as a risk factor for Alzheimer’s disease and the accumulation of proteins such as amyloid and tau. In earlier studies involving mice that were genetically predisposed to the amyloid and tau accumulation typical of Alzheimer’s disease, they found that sleep deprivation exacerbated this buildup. The latest study revealed that enhancing sleep in these mice with lemborexant appeared to offer protection, resulting in reduced tau protein tangles and decreased neuron death linked to Alzheimer’s disease.
The tau protein builds up in the brain across various neurological disorders, including Alzheimer’s, leading to inflammation and neuronal death. Holtzman and his team—co-led by first author Samira Parhizkar, PhD, an instructor in neurology—examined lemborexant partly because it affects areas of the brain known to be influenced by abnormal tau build-up. Additionally, it does not impair motor coordination, which is a concern for individuals with dementia taking sedative sleep medications.
Lemborexant is one of three sleep medications approved by the Food and Drug Administration that obstruct the effect of orexins, small proteins that modulate sleep, by serving as orexin receptor antagonists. Lemborexant inhibits both orexin receptors (type 1 and type 2). Receptors are proteins located on the cell surface that bind to other molecules and regulate cellular activities. These receptors are recognized for their vital roles in sleep-wake cycles and appetite, along with other physiological functions.
The pharmaceutical firm Eisai supplied lemborexant for these investigations as part of a research partnership with WashU Medicine aimed at advancing innovative treatments for Alzheimer’s disease, Parkinson’s disease, and additional neurodegenerative disorders.
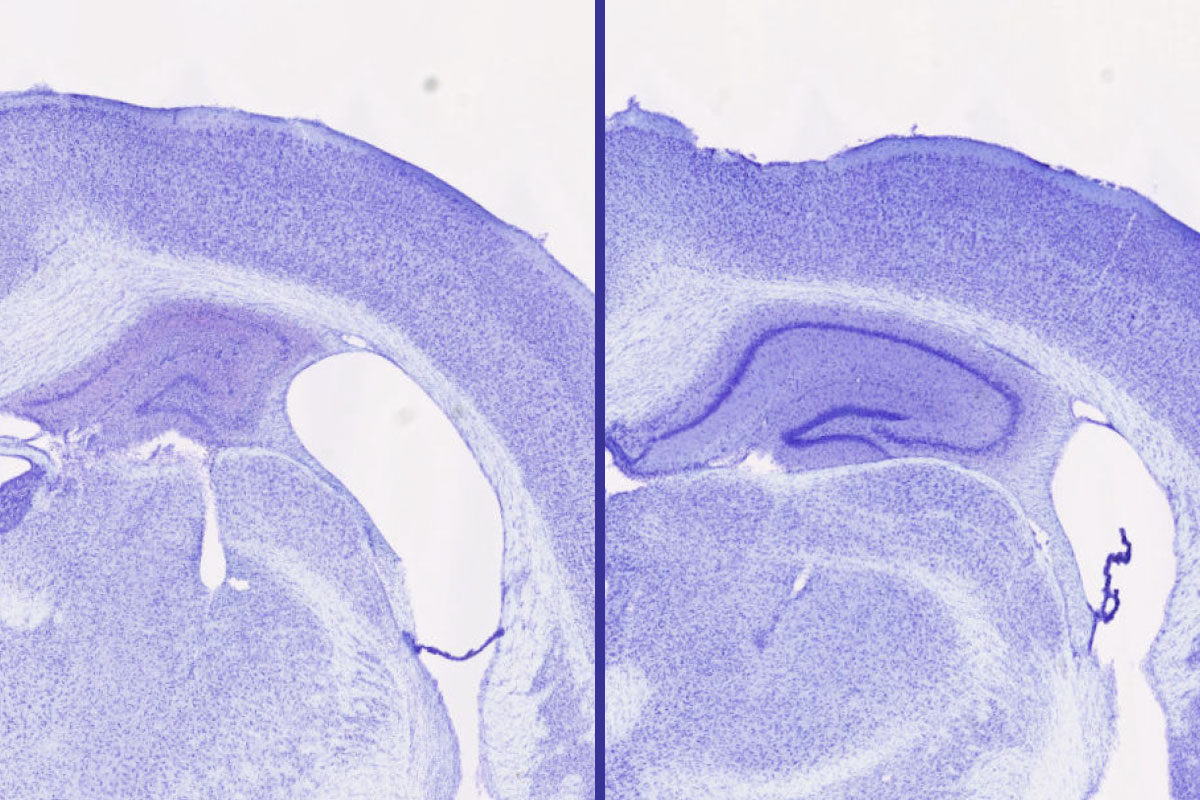
In mice genetically inclined to harmful tau accumulation, lemborexant mitigated brain damage compared to control mice. For instance, those receiving lemborexant exhibited a 30% to 40% greater volume in the hippocampus—a brain region critical for memory formation—relative to control mice and those treated with a different sleep medication, zolpidem, from an alternative drug class. Zolpidem enhanced sleep but lacked the protective benefits against tau accumulation in the brain observed with lemborexant, implying that the type of sleep aid—orexin receptor antagonist—is crucial in fostering neuroprotective effects. The researchers also noted that the positive effects were only evident in male mice, which they are still striving to comprehend.
Normal tau is essential for maintaining the architecture and function of neurons. When healthy, it carries a limited number of chemical markers known as phosphate groups. However, when tau acquires an excess of these chemical markers, it can aggregate, leading to inflammation and neuronal death. The authors discovered that by blocking orexin receptors, lemborexant prevents additional markers from being attached to tau, enabling tau to preserve its healthy functions in the brain.
Holtzman indicated that his team is continuing to investigate the reasons why the neuroprotective effects of lemborexant treatment were observed only in male mice. He speculated that the sex difference could be related to the observation that female mice with the same genetic tendency for tau accumulation exhibited less severe neurodegeneration compared to their male counterparts. With lesser damage initially, the potential benefits of the drug might have been subtler and more challenging to detect.
Parhizkar S, Bao X, Chen W, Rensing N, Chen Y, Kipnis M, Song S, Gent G, Tycksen E, Manis M, Lee C, Remolina Serrano J, Bosch ME, Franke E, Yuede CM, Landsness EC, Wong M, Holtzman DM. Lemborexant alleviates tau-mediated sleep loss and neurodegeneration in males in a mouse model of tauopathy. Nature Neuroscience. May 27, 2025. DOI: 10.1038/s41593-025-01966-7
This research was supported by the National Institutes of Health (NIH), grant numbers P01NS074969, RF1NS090934 and RF1AG061776; the JPB Foundation; the Alzheimer’s Association, grant number AARF-21-850865; the Rainwater Foundation, and a COBRAS Feldman Fellowship.
Holtzman is listed as an inventor on a patent licensed by Washington University to C2N Diagnostics regarding the therapeutic application of anti-tau antibodies. Holtzman co-founded and serves on the scientific advisory board of C2N Diagnostics.
About Washington University School of Medicine
WashU Medicine is a prominent authority in academic medicine, inclusive of biomedical research, patient healthcare, and educational programs with 2,900 faculty members. Its National Institutes of Health (NIH) research funding portfolio ranks as the second largest among U.S. medical schools, having expanded by 56% over the past seven years. Alongside institutional investment, WashU Medicine allocates over $1 billion annually to innovation and training in basic and clinical research. Its faculty practice consistently ranks among the top five nationally, with over 1,900 faculty physicians serving at 130 locations, who also work as the medical staff at Barnes-Jewish and St. Louis Children’s hospitals under BJC HealthCare. WashU Medicine boasts a rich history in MD/PhD training, having recently invested $100 million in scholarships and curriculum enhancement for its medical students, and is home to exemplary training programs across all medical subspecialties, as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website
The post Sleep aid halts neurodegeneration in mice appeared first on The Source.