“`html
When it pertains to inquiries regarding fungal infections, Andrej Spec, MD, has established himself as the primary authority for healthcare professionals globally. Weekly, he receives 10 to 15 inquiries from doctors grappling with intricate fungal diagnostics or treatment concerns. He has addressed questions from all over the U.S. and as far away as China, Thailand, Japan, Australia, and Europe.
“The issue is that a significant number of physicians were educated to perceive fungal infections as local and uncommon,” stated Spec, an associate professor of medicine in the Division of Infectious Diseases. “Consequently, when patients present with symptoms of an infection, they often do not contemplate the possibility of a fungus until every other option is exhausted.”
This medical oversight can lead patients with fungal infections on extensive and exasperating diagnostic journeys that extend illnesses and deteriorate outcomes. The WashU Medicine Invasive Fungal Infections Clinic, established in 2015, is making substantial progress in shortening that journey and offering top-notch diagnostics and care for this frequently overlooked category of infectious diseases. In its initial decade, the clinic has expanded from one specialist seeing three or four patients weekly to a thriving practice with three physicians, 1,200 patient visits annually, and a global reputation that has attracted patients from 37 U.S. states and five countries. Last year, the clinic was honored as a Center of Excellence, Diamond Level, by the European Confederation of Medical Mycology. It is among only 13 clinics worldwide to attain this acknowledgment and one of just two in the U.S. The other is at MD Anderson Cancer Center, which exclusively treats MD Anderson patients and does not accept referrals.
“Achieving this recognition is not straightforward,” remarked Spec, the founding director of the WashU Medicine fungal clinic. “You must exhibit excellence in three domains: diagnosis and testing; patient management; and research. Patients arrive here when all other options have been exhausted.”
Overcoming scopulariopsis

St. Louis resident Jonathan Ferretti, now 22, considers himself fortunate that the WashU Medicine fungal clinic was in proximity when he contracted one of the rarest and most fatal fungal infections. In 2020, while undergoing treatment for aggressive leukemia at St. Louis Children’s Hospital, black spots began emerging on his body—initially on his knee, then on his back. Successfully treating Ferretti’s leukemia required targeting the same immune cells that fend off infections, and the black spots immediately drew the attention of Ferretti’s care team, including WashU Medicine pediatric oncologist, Shalini Shenoy, MD, and WashU Medicine pediatric infectious disease expert, Rachel Orscheln, MD. Both physicians are professors of pediatrics treating patients at St. Louis Children’s Hospital.
They summoned Spec for an assessment of the patient, and he arrived at the diagnosis: the spots were induced by Scopulariopsis, a soil fungus that exploited Ferretti’s weakened immune system to invade his bloodstream and disseminate throughout his body.
At that time, only a handful of cases of disseminated scopulariopsis disease—indicating disease that had propagated throughout the body—had been documented in medical literature. All had resulted in fatalities.
“By the time I encountered scopulariopsis, I had already undergone chemotherapy, radiation, intubation, and a stem-cell transplant for leukemia,” Ferretti expressed. “My thought process had become so warped by cancer treatment that I didn’t comprehend the severity of this fungus. I perceived it as just another hurdle I had to clear.”
Prior to Ferretti starting intensive cancer treatment, his doctors had prescribed, as a precaution, three of the leading antifungal medications to diminish the risk of such infections, but none proved effective against the scopulariopsis overtaking his body. With no FDA-approved treatments specifically for disseminated scopulariopsis and the infection advancing swiftly, Spec identified that Ferretti’s sole chance of survival was participating in a clinical trial for the experimental antifungal agent olorofim, developed by the biotech company F2G. Spec and his team hurried to enroll Ferretti in the trial and administer the drug.
Within weeks, the spots started to vanish, although it took over a year for Spec to feel assured about discontinuing the drug. The trial has since concluded, and F2G is in the process of seeking FDA approval for olorofim.
“When Dr. Spec informed me that I might be the first person to survive disseminated scopulariopsis, I was astounded,” Ferretti recounted. “I still find it hard to believe.”
Broadening expertise beyond WashU Medicine
Ferretti is one of thousands of individuals whose lives have been impacted by the Invasive Fungal Infections Clinic. The clinic has established its reputation on delivering advanced diagnostics and cutting-edge treatment for various fungal infections, but its specialty lies in Histoplasma, a soil fungus that leads to histoplasmosis, an infection presenting flu-like symptoms such as fever, cough, and chills. However, histoplasmosis is significantly more lethal than the flu. Overall, the fungus claims around 5% of those infected, and the mortality rate escalates to 30% or higher for individuals with compromised immune systems.
This mold is found globally, but its primary hotspot is situated right in the Midwest, where WashU Medicine physicians and researchers have cultivated internationally recognized expertise in diagnosing and managing histoplasmosis. The WashU Medicine clinic is also home to what may be the only multidisciplinary care team specializing in a rare but critical and chronic complication of histoplasmosis called fibrosing mediastinitis. In this condition, abnormal tissue growth in the chest can result in blockages of airways, blood vessels, and the esophagus.
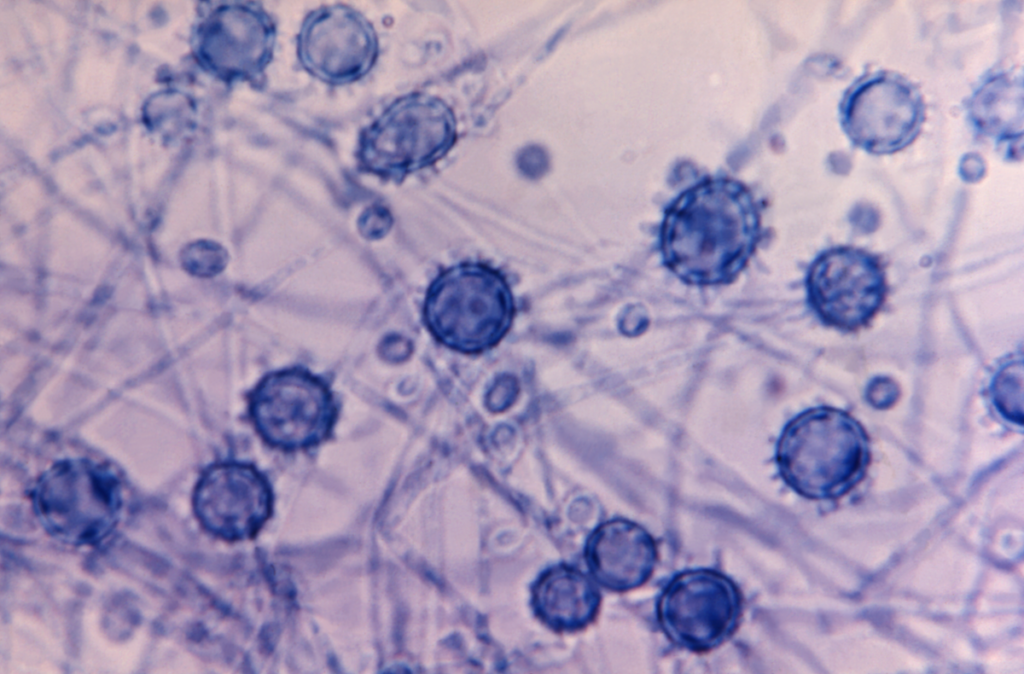
In addition, the clinic engages in several clinical trials for various fungal infections. These trials may provide access to experimental medications for patients who have exhausted approved options. The clinic’s physicians also conduct research on fungal infections, concentrating on Cryptococcus, Histoplasma, Candida, Aspergillus, and other invasive molds, including their epidemiology.
“““html
infections and elements that influence outcomes in individuals afflicted.
Many individuals suffering from invasive fungal infections encounter at least one erroneous diagnosis and ineffective treatment; on a national scale, the average number of misdiagnoses among patients with fungal infections is four. Adriana Rauseo, MD, an assistant professor of medicine and a member of the clinical staff at the fungal clinic, is striving to reduce the diagnostic pathway for patients by informing primary-care practitioners on recognizing fungal infections.
“To decrease the occurrence of misdiagnoses, we must enhance the awareness of fungal infections beyond just infectious disease specialists,” Rauseo stated. “We need primary-care providers to begin to ‘consider fungi.’ I’m not sure if it’s realistic to expect that individuals will be diagnosed correctly on the first attempt. However, receiving a diagnosis by the second visit to the physician is far better than the fifth. The strategy is to start with local practitioners and then broaden our reach.”
As WashU Medicine hosts the fungal clinic, it is one of the limited places offering rigorous training in diagnosing and managing invasive fungal infections. Infectious disease fellows from other institutions occasionally rotate through WashU Medicine specifically to train at the fungal clinic.
The medical field must rapidly update its knowledge about fungi, as conditions may be deteriorating. A 2022 study by Spec and colleagues indicated that lung infections caused by environmental fungi — previously confined to specific regions of the U.S. — have emerged as a nationwide concern due to certain species of pathogenic fungi venturing outside their traditional habitats in recent decades, likely influenced by climate change.
What’s worse, new fungal pathogens are on the verge of appearing, Spec warns. Numerous fungi residing in soil, water, and air possess the necessary molecular mechanisms to cause disease in humans but do so infrequently, mainly because they are suited for cooler conditions and struggle at human body temperature. However, with climate warming leading to prolonged and intensified heat waves, environmental fungi face pressure to acclimatize to elevated temperatures. Fungi may take a detrimental turn in a heated planet.
Collaborations with patients enhance care
Patrick B. Mazi, MD, an assistant professor of medicine and the third member of the fungal clinic staff, is involved with the fungal patient advocacy organization Mycology Advocacy, Research & Education, abbreviated as MyCARE. Co-founded by Spec in 2023 alongside patient activist Rob Purdie and medical education expert Lisa Tushla, MyCARE aims to enhance diagnosis and treatment of fungal infections by promoting awareness, aiding patients and caregivers, and advocating for increased and improved research.
“Rob Purdie often remarks, ‘I was diagnosed with a 50-year-old test and am being treated with a 70-year-old medication. In no other medical condition would that sentence be deemed acceptable,’” Mazi noted. “He’s correct! To effectively manage invasive fungal infections, we require improved diagnostics and treatments, which necessitates research.”
Clinical mycology, the scientific exploration and management of fungal infections, is significantly underfunded relative to other medical fields, compelling fungal researchers to be inventive. They are seeking insights from patients like Purdie to steer their research towards areas that will most positively influence patients’ lives.
“I must confess I was somewhat taken aback when I first conversed with patients and caregivers about their priorities,” Mazi expressed. “I was under the impression that superior treatments would be everyone’s primary concern. However, many patients emphasize the necessity for enhanced diagnostics so they could have been recognized and treated promptly. This revealed that their interactions during the initial phase of their fungal infection experience were so distressing that, even years later, they would favor improving that process for subsequent patients over finding better treatments for themselves.”
Currently, Ferretti is a relatively healthy 22-year-old university student aspiring to become a pediatric oncology nurse. He still faces some residual effects from his cancer treatment but has fully recuperated from his encounter with one of the most lethal fungi globally. He and his mother were present at MyCARE’s inaugural meeting in May 2023 in Denver, Colorado, where one of the co-founders is situated.
“This conference broadened my understanding of what fungal infections are truly capable of,” Ferretti shared. “It was genuinely frightening. Some individuals endured so much before receiving the care they needed. Even though I personally battled an invasive fungal infection, I didn’t fully grasp the severity until I attended that conference. I suppose I’m fortunate because I had Dr. Spec on my side from the outset. He literally saved my life.”
About Washington University School of Medicine
WashU Medicine is a prominent entity in academic medicine, covering biomedical research, patient care, and educational programs with a faculty of 2,900. Its National Institutes of Health (NIH) research funding portfolio ranks second among U.S. medical schools and has experienced a 56% growth over the past seven years. Coupled with institutional investments, WashU Medicine dedicates well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice consistently ranks among the top five in the nation, with over 1,900 faculty physicians practicing across 130 locations and serving on the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals under BJC HealthCare. WashU Medicine boasts a distinguished history in MD/PhD training, recently allocating $100 million to scholarships and curriculum enhancement for its medical students, and is home to exceptional training programs in every medical subspecialty alongside physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website
The post WashU Medicine fungal specialists combat frequently misdiagnosed infections appeared initially on The Source.
“`

