“`html
Envision a scenario where physicians could accurately fabricate tiny capsules capable of administering cells essential for tissue regeneration precisely where they are required within a pulsating heart. A consortium of researchers spearheaded by Caltech has made a notable advancement towards that overarching objective by devising a technique for 3D printing polymers at specific sites deep inside living organisms. This method utilizes acoustic waves for localization and has already been applied to generate polymer capsules for targeted drug delivery, as well as adhesive polymers for closing internal injuries.
Historically, researchers have relied on infrared light to initiate polymerization, which is the process of linking the fundamental units, or monomers, of polymers within live subjects. “However, the penetration of infrared is quite restricted. It only penetrates just beneath the skin,” states Wei Gao, professor of medical engineering at Caltech and an investigator at the Heritage Medical Research Institute. “Our novel approach penetrates deeper tissues and can fabricate various materials for a wide array of uses, all while ensuring remarkable biocompatibility.”
Gao and his team present their innovative in vivo 3D-printing technique in the journal Science. In addition to bioadhesive gels and polymers for drug and cell delivery, the article also elucidates the application of the technique to fabricate bioelectric hydrogels, which are polymers containing conductive materials intended for internal monitoring of vital physiological signs similar to electrocardiograms (ECGs). The primary author of the study is Elham Davoodi, an assistant professor of mechanical engineering at the University of Utah, who completed the research while serving as a postdoctoral fellow at Caltech.
The Genesis of a Unique Concept
Aiming to discover a method to achieve deep tissue in vivo printing, Gao and his colleagues investigated ultrasound, a technology widely utilized in biomedical applications for penetrating deep tissues. Yet, they required a strategy to activate crosslinking, or the binding of monomers, at designated sites only when necessary.
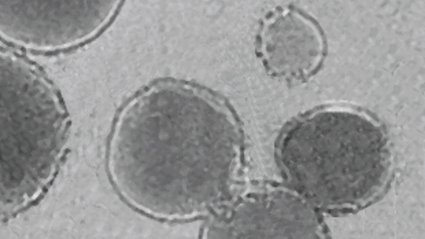
They devised a groundbreaking strategy: Integrate ultrasound with low-temperature-sensitive liposomes. These liposomes, spherical vesicles resembling cells and enveloped in protective lipid layers, are commonly utilized for drug delivery. In the current study, the researchers incorporated a crosslinking agent into the liposomes and embedded them within a polymer mixture containing the monomers of the polymer they intended to print, an imaging contrast agent to indicate when crosslinking occurred, and the therapeutic agent they aimed to deliver—a medication, for instance. Additional elements, such as cells and conductive materials like carbon nanotubes or silver, can also be added. The resulting bioink composite was subsequently injected directly into the organism.
Elevate the Temperature Slightly to Trigger Printing
The liposome particles demonstrate sensitivity to low temperatures, meaning that by utilizing focused ultrasound to increase the temperature of a small targeted area by roughly 5 degrees Celsius, the researchers can evoke the release of their payload and initiate the polymer printing process.
“Raising the temperature by a few degrees Celsius is sufficient for the liposome particles to release our crosslinking agents,” remarks Gao. “Wherever the agents are discharged, that’s where localized polymerization or printing will occur.”
The team employs gas vesicles derived from bacteria as an imaging contrast agent. These vesicles, air-filled protein capsules, prominently appear in ultrasound imaging and are responsive to chemical alterations that occur when the liquid monomer mixture crosslinks to form a gel network. The vesicles actually modify contrast, as detected via ultrasound imaging, when the transformation takes place, thereby allowing researchers to easily identify precisely when and where polymerization crosslinking has happened, facilitating the customization of patterns printed within living organisms.
This innovative technique has been dubbed the deep tissue in vivo sound printing (DISP) platform.
When the researchers employed the DISP platform to fabricate polymers infused with doxorubicin, a chemotherapy agent, adjacent to a bladder tumor in mice, they observed significantly greater tumor cell death over several days compared to animals that underwent direct drug solution injections.
“We have demonstrated in a small animal model that we can print drug-laden hydrogels for tumor therapy,” Gao states. “Our next step is to attempt printing in a larger animal model, and we are hopeful that soon we can evaluate this in human subjects.”
The team also envisions that machine learning can improve the DISP platform’s capacity to accurately locate and apply focused ultrasound. “In the future, with AI assistance, we aspire to autonomously initiate high-precision printing within a moving organ like a beating heart,” Gao predicts.
Additional contributors to the paper, “Imaging-guided deep tissue in vivo sound printing,” include Caltech graduate scholars Jiahong Li (MS ’23), Xiaotian Ma (MS ’24), Sunho Lee, and Jee Won Yang (MS ’23); Alireza Hassani Najafabadi, Ali Khademhosseini, and Hossein Montazerian from the Terasaki Institute for Biomedical Innovation in Los Angeles; Gengxi Lu, Yushun Zeng, and Qifa Zhou from USC; Jason Williams, Shervin S. Nia, Tzung K. Hsiai, and Paul S. Weiss from UCLA; Jounghyun Yoo, a visiting scholar in medical engineering at Caltech; Gwangmook Kim, a postdoctoral fellow in medical engineering at Caltech; Lei S. Li (PhD ’19), currently at Rice University; Zhiyang Jin (PhD ’24), Behnam Sadri, and Ehsan Shirzaei Sani, former postdoctoral researchers at Caltech; Lihong V. Wang, Caltech’s Bren Professor of Medical Engineering and Electrical Engineering, and the Andrew and Peggy Cherng Medical Engineering Leadership Chair; Di Wu (PhD ’21), research scientist and director of the DeepMIC Center at Caltech; and Mikhail G. Shapiro, Caltech’s Max Delbrück Professor of Chemical Engineering and Medical Engineering and a Howard Hughes Medical Institute Investigator.
This research was made possible through funding from the National Institutes of Health, the American Cancer Society, the Heritage Medical Research Institute, and the Challenge Initiative at UCLA. Fluorescence microscopy was conducted at the Advanced Light Microscopy/Spectroscopy Laboratory and the Leica Center of Excellence at the California NanoSystems Institute at UCLA.
“`