Autoimmune disorders, which are believed to impact over 15 million individuals in the U.S., arise when the body reacts to erroneous immune-system signals, dispatching infection-fighting responders to confront threats that are nonexistent. Researchers have long comprehended how these false signals are activated, yet the subsequent phase of deploying the immune reaction has remained elusive.
Currently, researchers at Washington University School of Medicine in St. Louis and the Perelman School of Medicine at the University of Pennsylvania have pinpointed a critical element involved in initiating immune activity — and excessive activity. The scientists discovered a protein in cells that accelerates the release of infection-fighting substances. This protein, previously unrecognized for its function in the immune system, presents a potential target for treatments aimed at preventing hyperactive immune responses responsible for numerous debilitating conditions.
Their study was published online in Cell on February 12 and is set to be printed on March 20.
The research team, led by Jonathan Miner, MD, PhD, an associate professor of rheumatology and microbiology as well as a member of Penn’s Colter Center for Autoimmunity, alongside David Kast, PhD, an assistant professor in the Department of Cell Biology & Physiology at WashU Medicine, made this breakthrough by investigating a rare autoimmune condition known as STING-associated vasculopathy with onset in infancy (SAVI). This ailment is extremely uncommon, affecting one in every 1 million births. It results in the immune system attacking tissues in patients’ lungs and limbs, frequently leading to fatality before reaching adulthood.
Examining rare ailments where the fundamental cause is attributed to a singular mutation can not only unveil the biological function of the affected gene and the disruptions it causes but also shed light on more prevalent disorders.
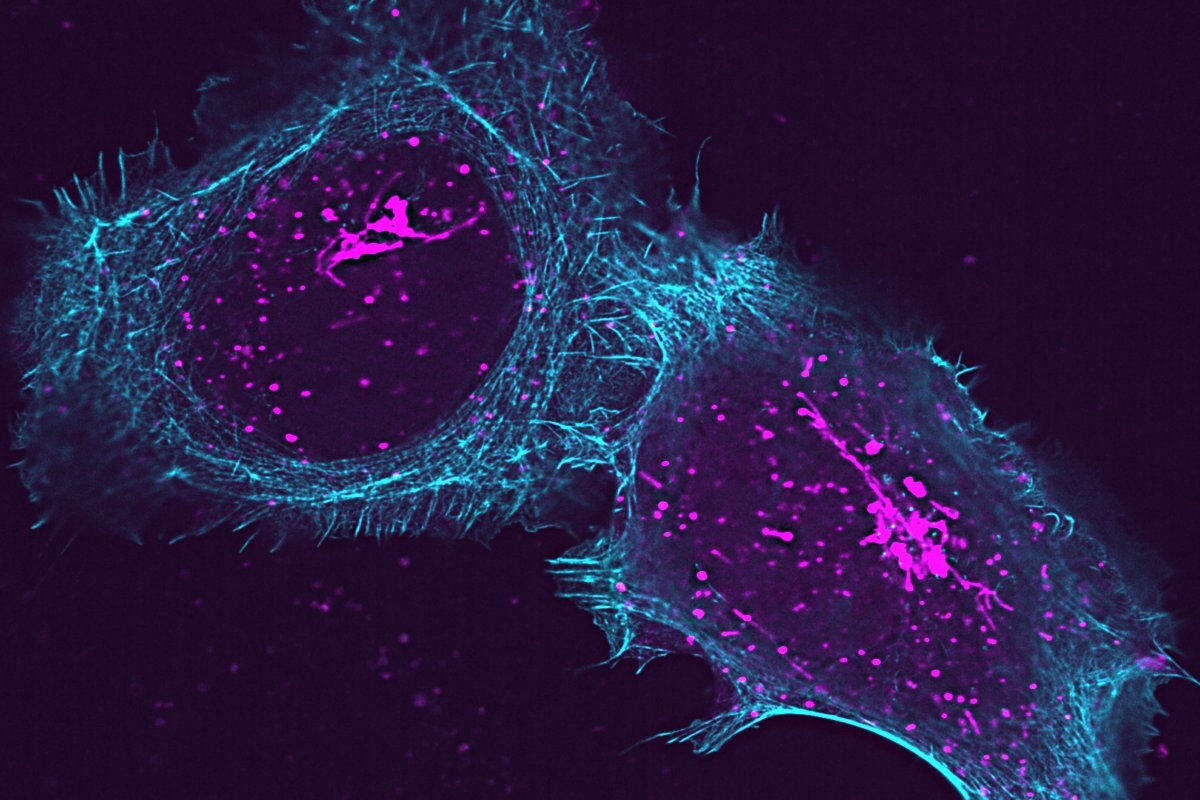
SAVI arises from alterations to a protein in cells called STING, which typically functions as a molecular sentinel that reacts to the presence of viral DNA by activating the part of the cell responsible for producing immune proteins. These immune proteins are released from the cell to alert the body’s immune system of the necessity to eliminate viral invaders and to indicate where in the body immune cells should be directed. In SAVI, STING is overly active, instigating persistent immune activity that ultimately harms healthy tissue.
Beyond signaling the cell to produce immune-response proteins, known as cytokines, the researchers discovered that STING also plays a unique role in releasing these proteins from their production sites within the cell. The mechanism of this release had not been understood, but controlling it could represent a promising strategy for treating SAVI and other autoimmune diseases.
Utilizing immune cells that were reactive to the disease-causing mutations in STING, the team conducted a screening process to find proteins that mitigated this sensitivity. One protein, ArfGAP2, emerged as significant, seemingly linked to the final phase of releasing the immune response proteins.
The researchers further confirmed this finding in SAVI cells lacking ArfGAP2. In its absence, STING was unable to trigger the release of the immune proteins.
“It’s akin to a train station, with ArfGAP2 serving as the conductor, directing which molecules are to be dispatched,” stated Kast. “Without collaboration between STING and ArfGAP2, the trains are stalled.”
The team hypothesized that halting the ceaseless “trains” in SAVI’s ongoing immune reaction could provide a pathway for treating the rare condition.
The team explored this concept in a mouse genetically modified to exhibit SAVI but lacking the ArfGAP2 protein. They found that the damaging immune response typical of the condition did not manifest, confirming that neutralizing the protein might cease the overactive immune response.
Miner, who began this project while at WashU Medicine, asserted that it is an encouraging target for other disorders that similarly lead to excessive production of related immune proteins. This may encompass the “cytokine storms” associated with COVID-19 or the brain inflammation connected to immune reactions in Alzheimer’s disease.
“Ailments like SAVI, which are quite rare, can offer significant insights,” stated Miner, “because if one can decipher how a rare disease mutation operates, knowledge is gained about the normal proteins present in all of us. This opens the door to numerous new possibilities for therapies across many different types of disorders.”
Poddar S, Chauvin SD, Archer CH, Qian W, Castillo-Badillo JA, Yin X, Disbennett WM, Miner CA, Holley JA, Naismith TV, Stinson WA, Wei X, Ning Y, Fu J, Ochoa TA, Surve N, Zaver SA, Wodzanowski KA, Balka KR, Venkatraman R, Liu C, Rome K, Bailis W, Shiba Y, Cherry S, Shin S, Semenkovich CF, De Nardo D, Yoh S, Roberson EDO, Chanda SK, Kast DJ, Miner JJ. ArfGAP2 promotes STING proton channel activity, cytokine transit, and autoinflammation. Cell, February 12, 2025. DOI: 10.1016/j.cell.2025.01.027
This research was funded by NIH grant numbers R01 AI143982, R01 436 NS131480, R01 GM136925, along with support from the Colton Center for Autoimmunity and the Clayco Foundation to J.J.M. The content represents solely the authors’ viewpoints and does not necessarily reflect the official opinions of the National Institutes of Health (NIH).
About Washington University School of Medicine
WashU Medicine is a prominent force in academic medicine, encompassing biomedical research, patient care, and educational initiatives with 2,900 faculty members. Its National Institutes of Health (NIH) research funding is the second highest among U.S. medical schools, having increased by 56% over the past seven years. Together with institutional support, WashU Medicine allocates well over $1 billion each year to fundamental and clinical research advancements and training. Its faculty practice continually ranks among the top five in the nation, featuring over 1,900 faculty physicians working at 130 sites and serving as the medical staff for Barnes-Jewish and St. Louis Children’s hospitals under BJC HealthCare. WashU Medicine boasts a distinguished history in MD/PhD education, having recently committed $100 million to scholarships and curriculum enhancements for its medical students, and hosts exceptional training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communication sciences.
Initially published on the WashU Medicine website
The post Researchers find missing link in autoimmune disorder appeared first on The Source.