Addressing severe or persistent damage to soft tissues like skin and muscle poses a significant challenge in the medical field. Existing treatment techniques can be expensive and often fall short of effectiveness. The incidence of chronic wounds, typically stemming from conditions like diabetes and vascular disorders, alongside a progressively aging demographic, is projected to increase.
A potentially effective treatment approach entails introducing biocompatible substances infused with living cells (i.e., microtissues) into the affected area. These materials offer a framework for stem cells or other precursor cells to proliferate into the damaged tissue and facilitate repair. Nonetheless, the existing methods for fabricating these scaffolding materials face a recurring challenge. Human tissue exhibits movement and flexibility in a distinctive manner that conventional soft materials fail to emulate; if the scaffolds expand, they can inadvertently stretch the embedded cells, often leading to cell death. This cell mortality obstructs the healing process and may also provoke an unintended immune reaction within the body.
“The human body possesses this hierarchical architecture that actually unfolds or un-crimps, rather than stretches,” remarks Steve Gillmer, a researcher in MIT Lincoln Laboratory’s Mechanical Engineering Group. “That’s the reason why if you stretch your own skin or muscles, your cells don’t perish. What’s occurring is your tissues are uncrimping slightly before undergoing stretching.”
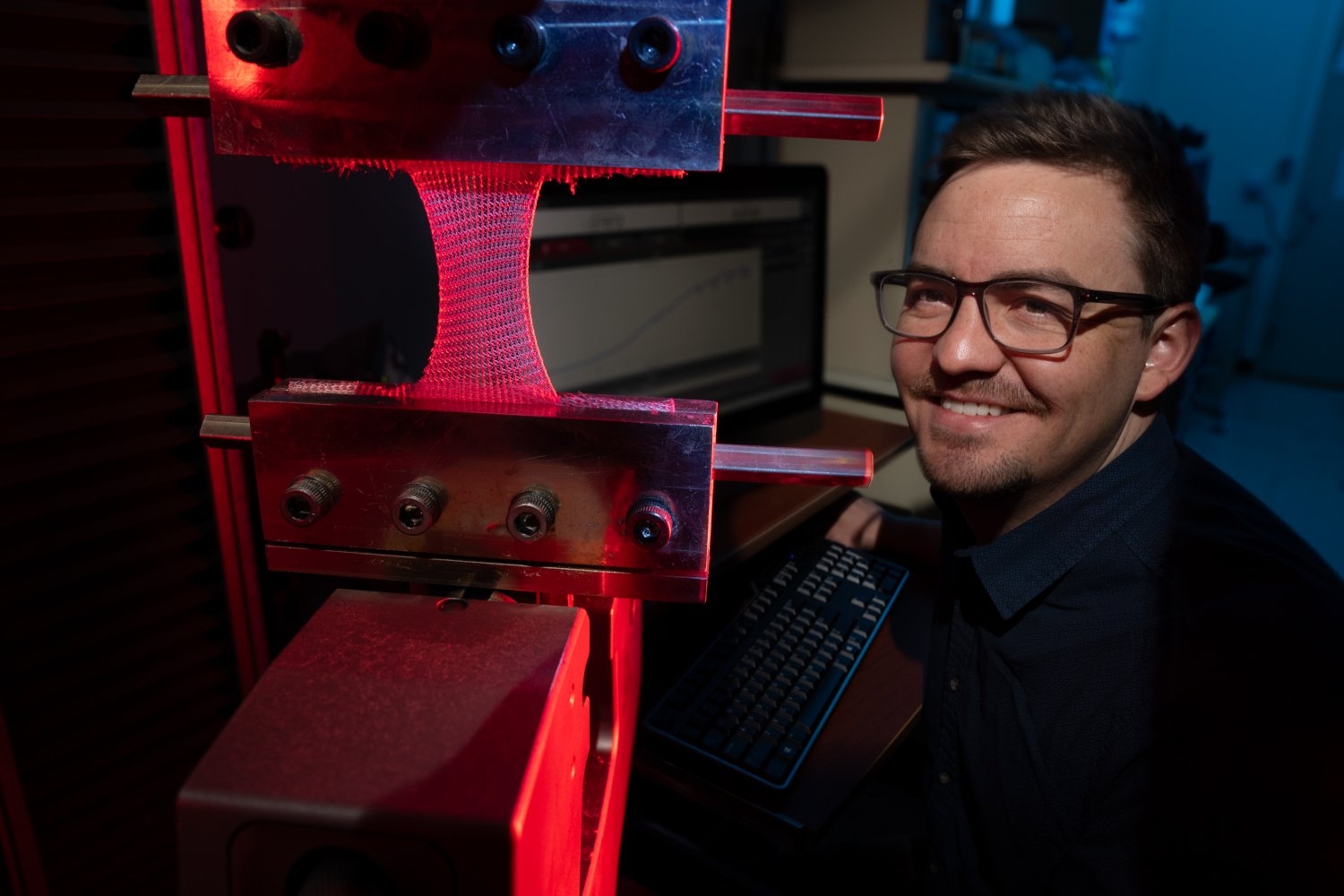
Gillmer is an integral member of a multidisciplinary research group that is on the quest to resolve this stretching challenge. He collaborates with Professor Ming Guo from MIT’s Department of Mechanical Engineering and the laboratory’s Defense Fabric Discovery Center (DFDC) to develop new types of textiles capable of uncrimping and moving in a manner identical to human tissue.
The initiative for the collaboration emerged during a course that Gillmer and Guo were co-teaching at MIT. Guo had been investigating methods to cultivate stem cells on innovative materials that could replicate the uncrimping nature of natural tissues. He opted for electrospun nanofibers, which demonstrated positive results but posed significant challenges in terms of fabrication length, hindering his ability to incorporate the fibers into larger knitting frameworks for extensive tissue repair.
“Steve pointed out that Lincoln Laboratory had access to industrial knitting machines,” Guo states. These machines allowed him to redirect his focus towards crafting larger knit designs instead of concentrating on individual yarns. “We promptly commenced testing new concepts with internal support from the lab.”
Gillmer and Guo collaborated with the DFDC to determine which knitting configurations could replicate the movement of various types of soft tissue. They initiated their work with three fundamental knitting styles known as interlock, rib, and jersey.
“For jersey, envision your T-shirt. When you pull on your shirt, the yarn loops are responsible for the stretching,” explains Emily Holtzman, a textile expert at the DFDC. “The longer the loop length, the greater the stretch your fabric can sustain. For ribbed, consider the cuff of your sweater. This fabric style has a global stretch that enables the fabric to unfold akin to an accordion.”
Interlock resembles ribbed but is knitted in a more compact pattern and contains double the amount of yarn per inch of fabric. By utilizing more yarn, there is an increased surface area available for embedding cells. “Knit fabrics can also be engineered to possess specific porosities or hydraulic permeability, formed by the loops and yarn sizes,” mentions Erin Doran, another textile expert on the team. “These pores can facilitate the healing process as well.”
Thus far, the team has performed numerous tests embedding mouse embryonic fibroblast cells and mesenchymal stem cells in various knitting patterns and observing their behavior when the patterns are stretched. Each pattern demonstrated variations that influenced how much the fabric could uncrimp and how rigid it became after stretching commenced. All patterns exhibited a high survival rate of cells, and in 2024 the team was honored with an R&D 100 award for their knitting designs.
Gillmer clarifies that although the project initially targeted skin and muscle injuries, their fabrics possess the capability to emulate many different forms of human soft tissue, including cartilage and fat. The team has recently submitted a provisional patent detailing the process of creating these patterns and identifying suitable materials for producing the yarn. This data can be utilized as a toolbox to adjust different knitted constructions to align with the mechanical attributes of the injured tissue they aim to support.
“This project has undoubtedly been an enlightening experience for me,” Gillmer asserts. “Each segment of this team brings a distinct area of expertise, and I believe the project would be unachievable without the collective effort. Our collaboration as a unified group allows us to broaden the scope of our work to address these larger, more intricate issues.”