“`html
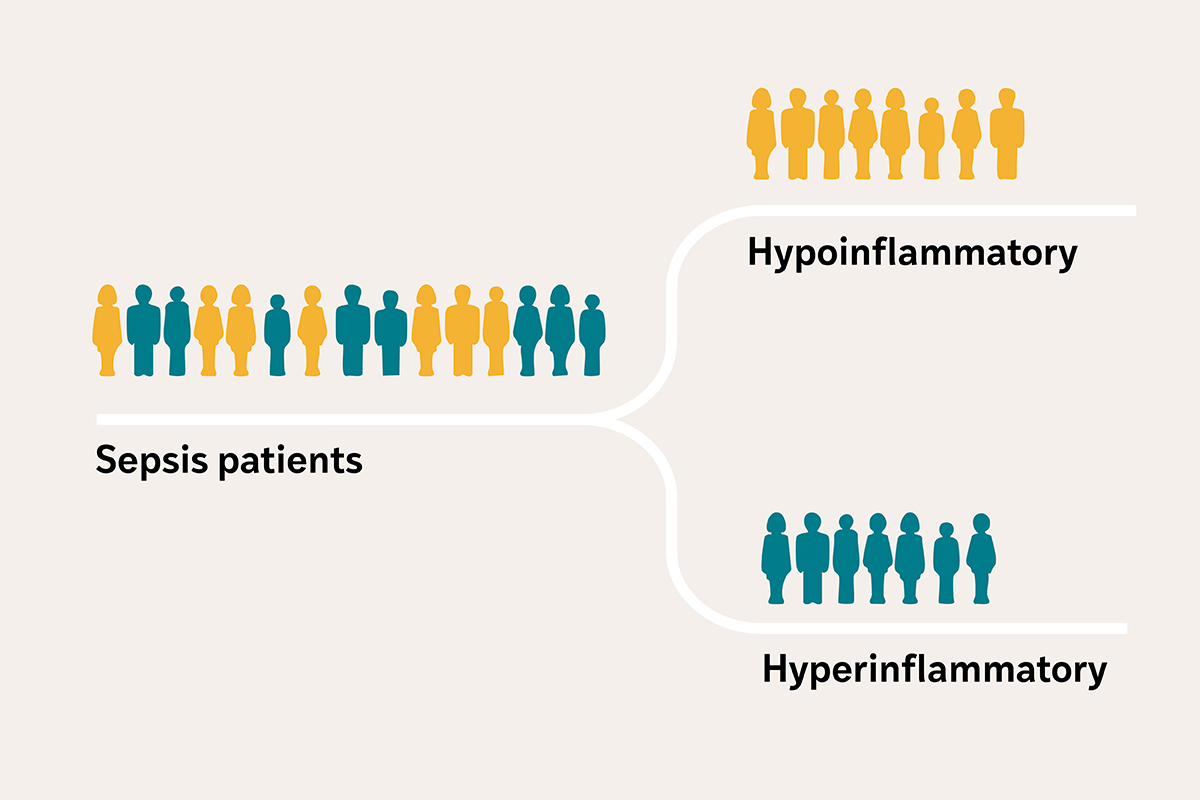
Severely ill individuals afflicted with sepsis — a disorder where the body’s reaction to an infection escalates uncontrollably and may result in organ harm — frequently enter the intensive care unit (ICU) exhibiting analogous symptoms, including fever, reduced blood pressure, and kidney dysfunction, among others. However, investigators at Washington University School of Medicine in St. Louis have unveiled that sepsis patients actually categorize into two separate profiles, determined by biological indicators present in their blood: one exhibiting intense inflammation and organ impairment, and the other showing a milder reaction.
Directing therapies toward these biological profiles could enhance the ability of doctors to address cases of sepsis more effectively, as per Pratik Sinha, MBChB, PhD, an assistant professor in the Department of Anesthesiology at WashU Medicine. Specifically, interventions previously considered ineffective may actually benefit patients with the severe inflammation profile. Yet, no clinical tools exist to rapidly and precisely differentiate these subsets, which have also been identified among individuals with other serious health conditions, such as acute respiratory distress syndrome, often triggered by sepsis, leading to profound lung failure.
A research group under Sinha’s leadership has secured a $4.87 million grant from the U.S. Department of Defense to formulate a clinical test and portable device designed to evaluate the levels of two biological markers in the blood, assisting physicians in swiftly categorizing sepsis patients into either a high-risk hyperinflammatory group or a less severe hypoinflammatory group.
“Creating an accurate test and a cost-effective device for the rapid identification of individuals with the high-risk hyperinflammatory profile is vital for administering targeted therapies and preserving lives in critical scenarios where prompt action is essential,” stated Sinha. “A compact device will facilitate use in active military and combat environments, where injuries heighten the likelihood of infection and sepsis.”
Patient subgroups may enhance sepsis management
Annually in the U.S., approximately 1.7 million individuals develop sepsis, with around 21% succumbing to the condition. This statistic includes military personnel suffering from serious infections due to combat-related trauma. The mortality rate surges to about 50% in patients exhibiting the hyperinflammatory profile of sepsis. Treatment involves antibiotics to combat the infection and supportive therapies for organs that have experienced damage, but this strategy overlooks a key component, according to Sinha.
“Existing treatments fail to address the body’s maladaptive reaction to the infection,” he remarked. “The key difficulty in providing effective treatments lies in the variation in the intensity of the biological response among individuals displaying similar symptoms.”
A preceding study involving 3,000 critically ill individuals conducted by Sinha and his associates, published in The Lancet Respiratory Medicine, established that the levels of two inflammatory cytokines — interleukin-8 (IL-8) and soluble tumor necrosis factor receptor 1 (sTNFR-1) — were dependable indicators of whether an individual had a high or low inflammatory response. Inflammatory cytokines are minor molecules that cells utilize for communication and can either enhance or alleviate inflammation.
Numerous therapies assessed in clinical trials involving the general sepsis patient demographic have been deemed ineffective, Sinha elaborated. However, when the researchers carried out a secondary analysis utilizing data from two earlier clinical trials and categorizing patients according to the two inflammatory profiles, they discovered that treatment effectiveness varied between the two factions. Dividing patients into subgroups to enrich clinical trials with participants sharing similar biological responses could potentially unlock fresh treatments and repurpose previously unsuccessful therapies to better the outcomes in sepsis and other critical illnesses.
Accurate, portable, and economical
Backed by this new funding, Sinha is partnering with Srikanth Singamaneni, PhD, the Lilyan & E. Lisle Hughes Professor at the McKelvey School of Engineering at WashU, to create a swift clinical test aimed at capturing IL-8 and sTNFR-1 from a few drops of plasma — the liquid part of blood that persists after blood cells have been eliminated — alongside a portable, handheld device to gauge the concentration of the captured proteins.
This proposed lateral flow test — akin to a COVID-19 rapid antigen test — would be the inaugural test to identify IL-8 and sTNFR-1 on a single strip. Unlike an at-home COVID-19 test that only indicates the presence of the SARS-CoV-2 virus, the researchers’ test integrates minute particles that emit light, referenced as plasmonic fluors, to measure the quantity of each inflammatory protein captured on the strip. The researchers will construct a device equipped with a camera to detect the luminescent particles, and a computational model will quantify levels to classify patients into the two subgroups.
“The biomarkers we aim to detect exist in very minuscule concentrations in the blood,” remarked Singamaneni, who developed the lateral flow system featuring plasmonic fluors. The plasmonic fluor technology has been patented and licensed to Brightest Bio, a WashU startup formerly known as Auragent BioSciences, by WashU’s Office of Technology Management. “Incorporating the fluorescent nanoparticles into the test enhances its sensitivity, allowing us not only to detect but also to accurately gauge these biomarkers,” Singamaneni continued. “Its sensitivity differentiates our test from other lateral flow assays and is critical for categorizing patients into groups.”
The researchers are working on the test and device to be economical, precise, and rapid. Its compact and portable design will facilitate deployment in various critical care environments, including military bases, combat areas, and rural hospitals.
“This instrument holds the potential to reach patients at their bedside, providing customized care based on each individual’s unique biological responses,” stated Sinha. “We aspire to address a critical need in acute care that will enable more effective treatments for a greater number of patients.”
The U.S. Army Medical Research Acquisition Activity, 808 Schreider Street, Fort Detrick MD 21702-5014 functions as the awarding and administering acquisition office. This initiative was backed by The Assistant Secretary of Defense for Health Affairs and endorsed by the Department of Defense, amounting to $4,876,076.00 through the Peer Reviewed Medical Research Program under Award Number HT9425-25-1-0825. Views, interpretations, conclusions, and recommendations are those of the author(s) and do not necessarily reflect the stance of the Department of Defense.
About Washington University School of Medicine
WashU Medicine is a prominent entity in academic medicine, encompassing biomedical research, patient treatment, and educational endeavors with 2,900 faculty members. Its National Institutes of Health (NIH) research funding profile ranks second largest among U.S. medical schools, having expanded by 83% since 2016. In conjunction with institutional investment, WashU Medicine allocates well over $1 billion annually to fundamental and clinical research innovation and training. Its faculty practice consistently ranks in the top five nationally, with more than 1,900 physician faculty operating at 130 locations. WashU Medicine physicians solely staff Barnes-Jewish and St. Louis Children’s hospitals — the academic hospitals of BJC HealthCare — and provide care at BJC’s community hospitals throughout the region. WashU Medicine boasts a rich history in MD/PhD training, having recently dedicated $100 million to scholarships and curriculum enhancements for its medical students, and hosts exemplary training programs in every medical subspecialty, along with physical therapy, occupational therapy, and audiology and communication sciences.
Originally published on the WashU Medicine website
The post $4.87 million grant supports development of sepsis diagnostic device appeared first on The Source.
“`