When harmed, cells exhibit well-coordinated reactions to facilitate recovery. These responses encompass a long-recognized process of self-destruction, which eliminates dead and damaged cells, alongside a newer phenomenon that aids older cells in reverting to a seemingly younger state to foster the regrowth of healthy tissue.
Now, a recent study involving mice, led by researchers from Washington University School of Medicine in St. Louis and the Baylor College of Medicine, discloses a previously unidentified cellular purging mechanism that may expedite the return of injured cells to a stem cell-like condition. The researchers have termed this newly uncovered response “cathartocytosis,” deriving from Greek root terms meaning cellular cleansing.
Published online in the journal Cell Reports, the investigation employed a mouse model of stomach injury to shed light on how cells heal or fail to heal in reaction to damage, such as from infections or inflammatory conditions.
“Following an injury, a cell’s role is to mend that damage. However, the cell’s developed machinery for executing its usual functions can obstruct this process,” stated first author Jeffrey W. Brown, MD, PhD, an assistant professor of medicine in the Division of Gastroenterology at WashU Medicine. “Thus, this cellular cleansing serves as a swift mechanism to dispose of that machinery, enabling it to quickly transform into a small, primitive cell capable of proliferating and repairing the injury. We identified this mechanism in the gastrointestinal tract, but we believe it is pertinent in other tissues as well.”
Brown compared this mechanism to a “vomiting” or expelling of waste, effectively providing a shortcut that assists the cell in decluttering and concentrating on regenerating healthy tissues more rapidly than it could if limited to a gradual, controlled degradation of waste.
Like many shortcuts, this one carries potential drawbacks: According to the researchers, cathartocytosis is swift but chaotic, which may illuminate how injury responses can malfunction, particularly in chronic injury scenarios. For instance, persistent cathartocytosis in reaction to an infection signifies chronic inflammation and ongoing cellular damage, creating a fertile environment for cancer. In fact, the accumulated mess of expelled cellular waste resulting from extensive cathartocytosis may also serve as a means to identify or monitor cancer, according to the researchers.
A novel cellular process
The researchers discovered cathartocytosis within a vital regenerative injury response known as paligenosis, which was first outlined in 2018 by the lead author of the current study, Jason C. Mills, MD, PhD. Now at the Baylor College of Medicine, Mills initiated this research while serving as a faculty member in the Division of Gastroenterology at WashU Medicine, with Brown as a postdoctoral researcher in his laboratory.
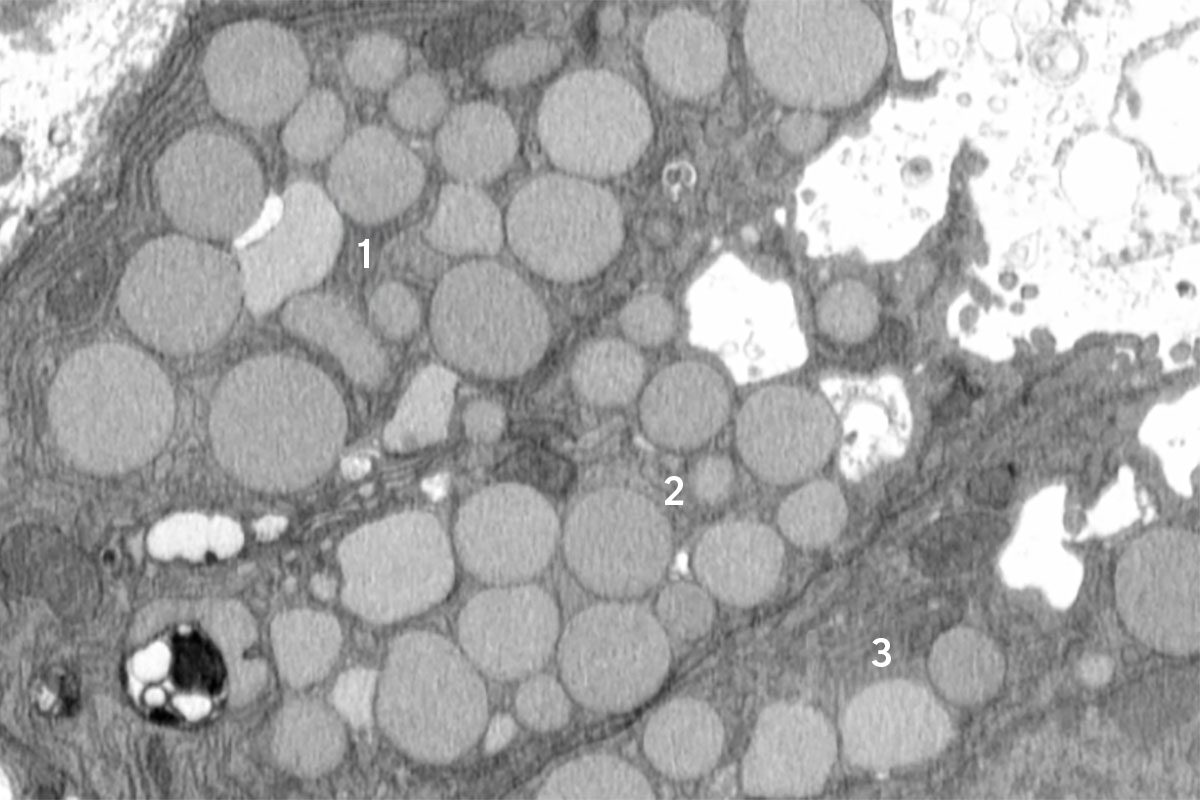
In paligenosis, injured cells diverge from their regular functions and undergo a reprogramming process toward an immature state, acting like rapidly multiplying stem cells, akin to what transpires during development. Initially, the researchers presumed that the decluttering of cellular machinery in preparation for this reprogramming took place entirely within cellular compartments called lysosomes, where waste is digested in a gradual and contained manner.
However, from the outset, the researchers detected debris outside of the cells. They initially overlooked this as insignificant, yet as they observed more external waste in their preliminary studies, Brown began to suspect that something intentional was occurring. He employed a model of mouse stomach injury that prompted the reprogramming of mature cells to a stem cell state all at once, making it evident that the “vomiting” response — now occurring in all stomach cells simultaneously — was a characteristic of paligenosis, rather than an anomaly. In other words, the vomiting process wasn’t simply an accidental spill but a newly recognized, standard response of cells to injury.
While they found cathartocytosis occurring during paligenosis, the researchers noted that cells might also utilize cathartocytosis to expel waste in other, more troubling situations, such as enabling mature cells to begin acting like cancer cells.
The drawback of downsizing
Although the recently uncovered cathartocytosis process may assist injured cells in progressing through paligenosis and regenerating healthy tissue more swiftly, the trade-off involves additional waste products that could exacerbate inflammatory states, complicating the resolution of chronic injuries and correlating with an elevated risk of cancer development.
“In these gastric cells, paligenosis — the return to a stem cell state for healing — presents a perilous process, especially now that we’ve recognized the potentially inflammatory downsizing of cathartocytosis involved,” Mills stated. “These stomach cells are long-lived, and aging cells accumulate mutations. If numerous older mutated cells revert to stem cell states in an attempt to repair an injury — and injuries frequently fuel inflammation, such as during an infection — there’s an increased risk of acquiring, perpetuating, and amplifying detrimental mutations that lead to cancer as those stem cells proliferate.”
Further study is warranted, but the authors suspect that cathartocytosis may contribute to prolonging injury and inflammation in Helicobacter pylori infections within the gut. H. pylori is a type of bacterium recognized for infecting and damaging the stomach, resulting in ulcers and heightening the risk of stomach cancer.
The insights gained could also indicate new therapeutic approaches for stomach cancer and potentially other gastrointestinal malignancies. Brown and his WashU Medicine collaborator Koushik K. Das, MD, an associate professor of medicine, have created an antibody that attaches to components of the cellular waste expelled during cathartocytosis, offering a method to detect when this process might be occurring, especially in substantial quantities. In this way, cathartocytosis might serve as a marker for precancerous conditions that could enable early identification and intervention.
“If we deepen our understanding of this process, we could devise methods to promote the healing response and perhaps, in the context of chronic injury, prevent damaged cells undergoing chronic cathartocytosis from contributing to cancer development,” Brown remarked.
Brown JW, Lin X, Nicolazzi GA, Liu X, Nguyen T, Radyk MD, Burclaff J, Mills JC. Cathartocytosis: expelling cellular material during reprogramming of differentiated cells. Cell Reports. Online July 20, 2025. DOI: 10.1016/j.celrep.2025.116070.
This research received support from the National Institutes of Health (NIH), grant numbers K08DK132496, R21AI156236, P30DK052574, P30DK056338, R01DK105129, R01CA239645, F31DK136205, K99GM159354, and F31CA236506; the Department of Defense, grant number W81XWH-20-1-0630; the American Gastroenterological Association, grant numbers AGA2021-5101 and AGA2024-13-01; as well as a Philip and Sima Needleman Student Fellowship in Regenerative Medicine. The views expressed are solely those of the authors and do not necessarily reflect the official opinions of the NIH.
About Washington University School of Medicine
WashU Medicine is a leading institution in academic medicine, including biomedical research, patient care, and educational initiatives with 2,900 faculty members. Its National Institutes of Health (NIH) research funding portfolio ranks as the second largest among U.S. medical schools and has increased by 83% since 2016. In conjunction with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently among the top five in the nation, with over 1,900 faculty physicians caring for patients at 130 locations. WashU Medicine doctors exclusively serve Barnes-Jewish and St. Louis Children’s hospitals — the educational hospitals of BJC HealthCare — and provide care at BJC’s community hospitals in the region. WashU Medicine has a distinguished history in MD/PhD training, recently allocating $100 million to scholarships and curriculum renewal for its medical students and is home to exemplary training programs in every medical subspecialty, as well as physical therapy, occupational therapy, and audiology and communications sciences.
Initially published on the WashU Medicine website
The post Cells ‘vomit’ waste to promote healing, mouse study reveals appeared first on The Source.