“`html
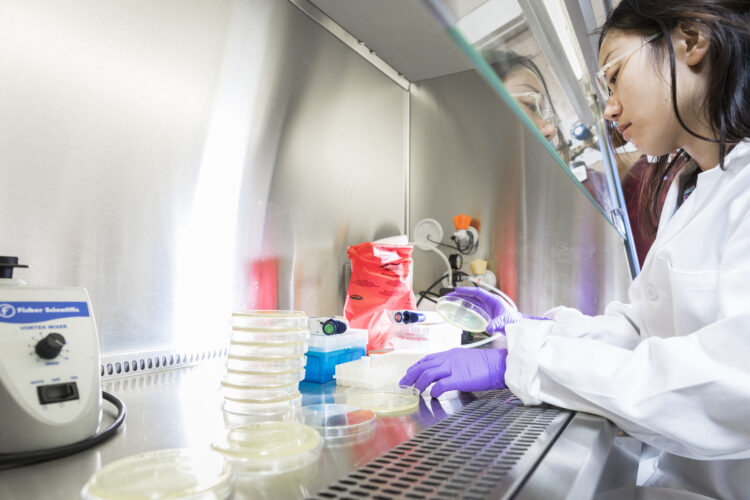
University of Washington researchers evaluated the effectiveness of several prevalent disinfectants against genes that confer antibiotic resistance in bacteria. Pictured here is lead author Huan He setting up agar plates for assessing bacterial inactivation in disinfection trials.Mark Stone/University of Washington
Antimicrobial resistance poses a persistent danger in medical facilities globally. As more bacteria and other microorganisms develop defenses against available medications, an increasing number of patients face the threat of contracting infections resistant to treatment.
Now, researchers at the University of Washington present fresh insights into strategies presently employed to mitigate the dissemination of antibiotic-resistant bacteria and other pathogens within healthcare settings.
In a recent publication in Environmental Science & Technology, the team scrutinized the effectiveness of nine widely-used disinfectants found in healthcare settings or households — including ethanol, hydrogen peroxide, benzalkonium chloride, and UV light — against three renowned strains of antibiotic-resistant bacteria. Initially, the researchers examined how effectively each disinfectant eliminated (or more precisely, “inactivated”) the bacteria.
Then the team advanced their investigation. They also analyzed the harm the disinfectants inflicted upon the root of the resistance: the bacterial genome itself. While all the disinfectants were effective in halting bacterial growth, the scenario changed significantly when focusing on DNA.
“What we’re discovering is that it’s not solely the bacteria we must contend with in hospitals and similar environments. It’s the behavior of their DNA in these contexts as well,” stated lead author Huan He, who conducted this research as a UW doctoral candidate in the civil and environmental engineering division and is currently an assistant professor at Tongji University.
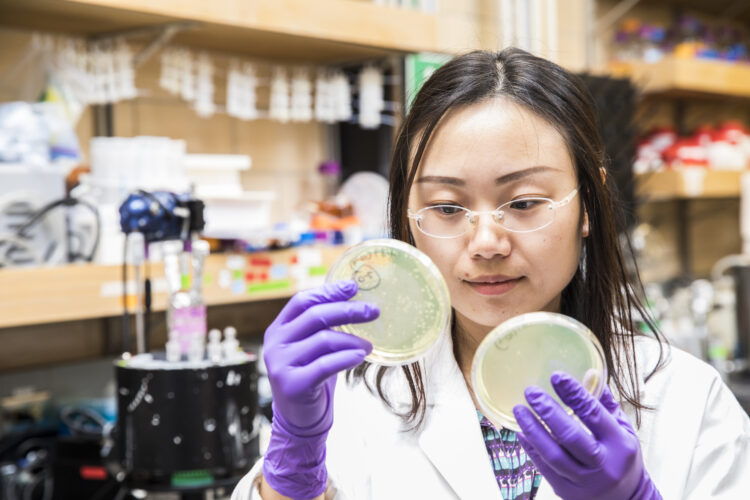
Lead author Huan He observes bacterial growth on agar plates before and following disinfection.Mark Stone/University of Washington
Within bacterial cells, the origin of antibiotic resistance lies in specific genes — distinct segments of DNA — that direct a cell to shield itself against particular antibiotics. Contemporary disinfectants excel at halting bacterial cells, but the genes of a bacterium might endure even after cell death. Moreover, due to a mechanism known as “horizontal gene transfer,” genes from a dead bacterium may occasionally transfer to a new living bacterium, perpetuating antibiotic resistance.
In essence, merely eliminating the bacteria is not always sufficient to halt the progression of resistance.
“Environmental engineers are increasingly regarding resistance genes as emerging contaminants,” remarked He. “In public health environments like hospitals, we might disinfect and sanitize an operating theater to eliminate bacterial contamination, but what if resistance genes persist? They could potentially infect other bacteria and lead to more severe antibiotic-resistant infections acquired in hospitals.
“Our past research has shown that resistance genes can remain active during horizontal transfer after water and wastewater disinfecting, prompting us to question whether similar situations could arise in healthcare and personal-care disinfection methods.”
The study tested the nine disinfectants against three varieties of antibiotic-resistant bacteria, including methicillin-resistant Staphylococcus aureus (MRSA), the organism responsible for severe staph infections. Researchers placed bacterial samples in varied settings, primarily as dried droplets on stainless steel and nonstick surfaces commonly found in medical facilities and homes. They then administered the disinfectants and evaluated the impacts on both bacterial cells and the relevant genes.
As anticipated, the disinfectants effectively halted bacteria. However, most exhibited little influence on the resistance-encoding genes. The DNA persisted largely unaltered, ready to transfer into new bacteria.
There were notable positive and negative outliers, often not the cleansers the team had predicted.
“Chlorine, under our testing conditions, appeared to be less effective against DNA than we initially expected, while another typical cleaner, phenol, which we anticipated would be ineffective, surprisingly demonstrated relatively favorable results in some circumstances,” noted senior author Michael Dodd, a UW associate professor in the civil and environmental engineering department.
The standout disinfectant in many of the trials was UV light, which inflicted considerable damage to the problematic genes — though ultimately less than what the team had hoped for.
“UV irradiation seems to be among the more effective methods for both inactivating bacteria and degrading their DNA,” Dodd remarked. “We know that UV light directly damages DNA, so we weren’t entirely surprised to see it excel in this context. Nonetheless, it was an encouraging outcome.”
The researchers promptly emphasized that current disinfection practices in hospitals are still vital and effective in preventing disease transmission.
Senior author Michael Dodd with Huan He.Mark Stone/University of Washington
This research can aid scientists in focusing on the methods that deliver the most effective dual approach against troubling bacteria and their genes. Looking ahead, the team aims to understand better how to optimize the effects of these disinfectants, particularly when incorporating variables like ambient temperature, humidity, and bacterial cell density. However, the findings from this study might already assist hospitals in refining their disinfection protocols.
“If you know a patient in a hospital or other healthcare facility is infected with an antibiotic-resistant pathogen, we now have enough evidence to suggest using certain disinfectants over others when cleaning surfaces or instruments the patient may have contacted,” Dodd indicated. “For instance, UV light could be a favorable option, while benzalkonium chloride may not be.”
Other co-authors on this study include Sin-Yi Liou, a former graduate researcher at UW.
“““html
who is currently a postdoctoral scholar at Gwangju Institute of Science and Technology; Kyle K. Shimabuku, a previous research assistant at UW who now holds the position of associate professor at Gonzaga University; Peiran Zhou, a former graduate researcher at UW who is presently a medical resident at the UW School of Medicine; Yegyun Choi, a past guest researcher at UW who is now a research professor affiliated with Gwangju Institute of Science and Technology; John S. Meschke, a faculty member at UW specializing in environmental and occupational health sciences; Marilyn C. Roberts, an emeritus professor at UW in environmental and occupational health sciences; and Yunho Lee, a professor at the Gwangju Institute of Science and Technology.
This study received funding from the National Science Foundation, the National Natural Science Foundation of China, the Fundamental Research Funds for the Central Universities, and the Allen & Inger Osberg Endowed Professorship.
For additional details, reach out to Michael Dodd at [email protected] and Huan He at [email protected]
“`
